Chapter: Essentials of Psychiatry: Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder: Course and Natural History
Course and Natural History
Age at Onset
Age at onset usually refers to the age when OCD symptoms (ob-sessions
and compulsions) reach a severity level wherein they lead to
impaired functioning or significant distress or are time-consuming (i.e., meet
DSM-IV criteria for the disorder). Reported age at onset is usually during late
adolescence. In one study drawn from an OCD clinic sample (N = 560), the onset for males
occurred significantly earlier than for females (19.5 ± 9.2 years versus 22.0 ± 9.8 years). In this study, 83%
of patients experi-enced the onset of significant symptoms between ages 10 and
24 years, whereas less than 15% experienced onset after age 35 years (Rasmussen
and Eisen, 1998). People with OCD, however, usu-ally describe the onset of
minor symptoms in childhood, well be-fore the onset of symptoms meeting full
criteria for the disorder.
In
several studies, earlier age at onset has been associated with an increased
rate of OCD in first-degree relatives and sug-gest that there is a familial
type of OCD characterized by early onset. Age at onset of OCD may also be a
predictor of course. The vast majority of patients report a gradual worsening
of obsessions and compulsions prior to the onset of full-criteria OCD, which is
followed by a chronic course (see later). However, Swedo and colleagues (1998)
have described a subtype of OCD that beginsbefore
puberty and is characterized by an episodic course with intense exacerbations.
Exacerbations of OCD symptoms in this subtype have been linked with Group A
beta-hemolytic strep-tococcal infections, which has led to the subtype
designation of pediatric autoimmune neuropsychiatric disorders associated with
streptococcal infections (PANDAS). In their study of 50 children with PANDAS,
the average age of onset was 7.4 years. Whether the course of illness in
patients with PANDAS continues to be episodic into adulthood, or, as is the
case with postpubertal on-set, tends to be chronic, is not known.
In
keeping with the older literature, a recent 2-year natu-ralistic prospective
study of 65 adults with OCD, in which the effect of treatment was assessed,
supported earlier findings that OCD is usually chronic with fluctuations in symptom
intensity but no lasting remission; it is notable that this course was most
common even during an era when effective treatments were avail-able. Although
50% of the subjects achieved partial remission in the first year of the study,
the probability of subsequent relapse was 48%. Only 12% achieved full and
sustained remission (Eisen et al., 1999). In contrast, a better outcome was found
in a follow-up study of 144 people with OCD assessed in the 1950s and again in
the 1990s (mean length of follow-up from illness onset was 47 years). Most
subjects reported a significant decrease in OCDsymptom
severity, which varied from complete recovery (20%), to recovery with continued
subclinical symptoms (28%), to con-tinued OCD but with clear improvement (35%).
Better outcome was associated with later age of onset and poorer social
function-ing at baseline (Skoog and Skoog, 1999).
In a prospective study of children with OCD, the major-ity (52%) of the
25 patients had moderate to severe OCD in the 2- to 7-year follow-up period
(Flament et al., 1990), which is
con-sistent with the data on adults. A more recent prospective study of 54 children
with OCD who were treated with clomipramine yielded a more hopeful picture of
OCD’s course. At 2 to 7 years after initial referral, 43 of these patients
still had symptoms that met criteria for OCD, but 73% were considered much or
very much improved, and 11% were completely asymptomatic (Leonard et al., 1993). This study suggested that
appropriate somatic treat-ment may improve outcome only while the patient
continues to receive this treatment (see later).
Phenomenology
OCD’s clinical presentation is characterized by phenomenological
subtypes based on the content of the obsessions and correspond-ing compulsions.
The list of subtypes in the Yale-Brown Obses-sive–Compulsive Scale (Y-BOCS)
(Table 51.1) was generated on
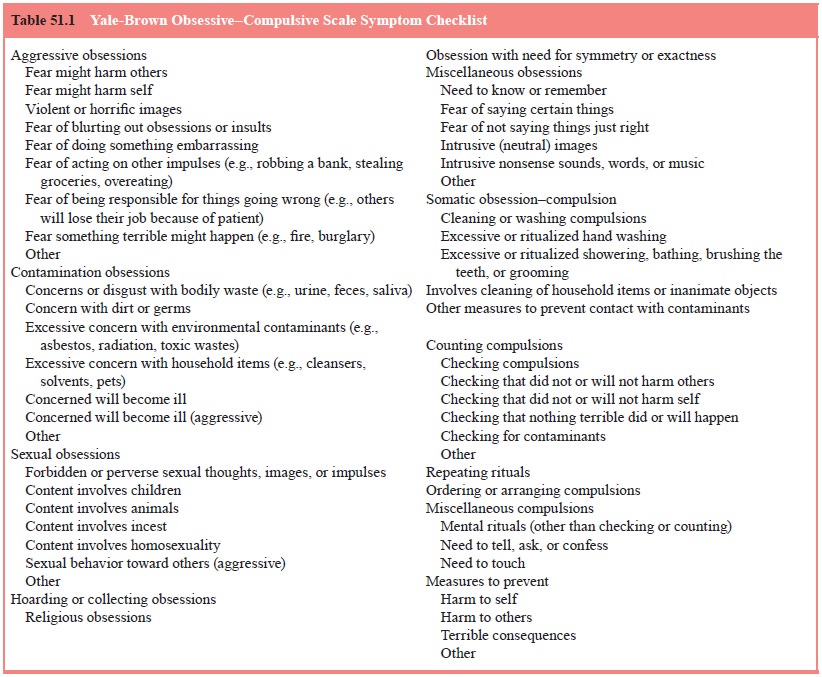
the basis of clinical interviews with OCD patients in the 1980s. These
subtypes are remarkably consistent with phenomenologi-cal descriptions in the
psychiatric literature beginning with scru-pulosity in the 15th century.
The basic types of obsessions and compulsions seem to be consistent
across cultures. The most common obsession is fear of contamination, followed
by pathological doubt, a need for symmetry and aggressive obsessions (Figure
51.1). The most common compulsion is checking, which is followed by washing,
symmetry, the need to ask or confess and counting (Figure 51.2). Children with
OCD present most commonly with washing com-pulsions, which are followed by
repeating rituals.
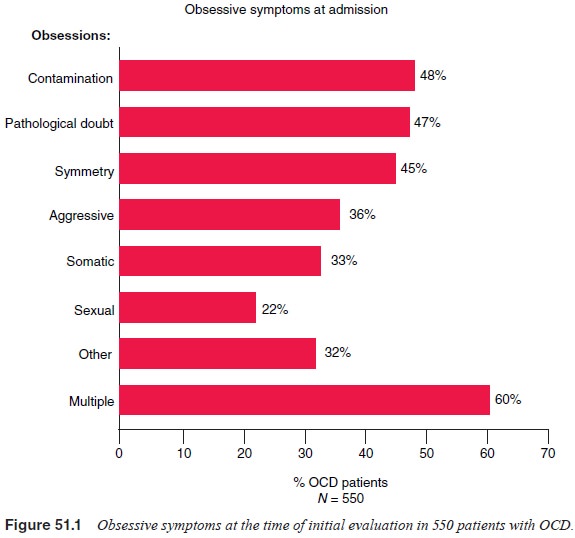
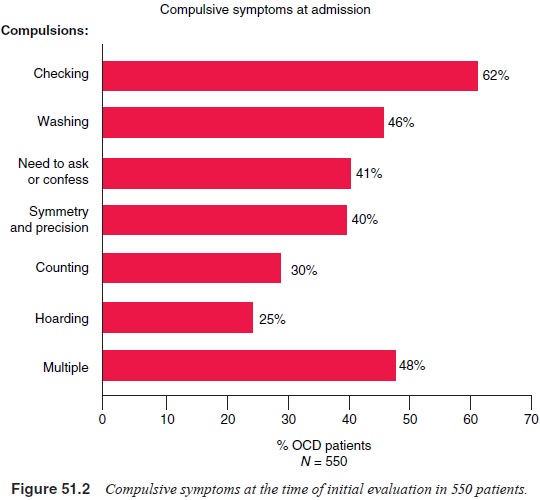
Most patients have multiple obsessions and compulsions over time, with a
particular fear or concern dominating the clini-cal picture at any one time.
The presence of obsessions without compulsions, or compulsions without
obsessions, is unusual. In the DSM-IV OCD field trial of 431 patients, only 2%
had pre-dominantly obsessions and 2% had predominantly compulsions; the
remaining 96% endorsed both obsessions and compulsions (Foa and Kozak, 1995).
Patients who appear to have obsessions without compulsions frequently have
unrecognized reassurance rituals or mental compulsions, such as repetitive,
ritualized pray-ing, in addition to their obsessions. Pure compulsions are also
unusual in adults, although they do occur in children, especially in the young
(e.g., 6 to 8 years of age). Most people have both mental and behavioral
compulsions; in the DSM-IV field trial 79.5% reported having both mental and
behavioral compulsions, 20.3% had behavioral compulsions only and 0.2% had only
men-tal compulsions.
The search for whether specific obsessions and compul-sions have
predictive value in terms of treatment response biologic markers, or genetic
transmission has not been particu-larly fruitful. There has been considerable
interest in exploring whether certain clusters of obsessions and compulsions
repre-sent specific OCD phenotypes. A number of studies have ad-dressed this
question systematically using the Y-BOCS Symp-tom Checklist to identify groups
of obsessions and compulsions that cluster together on factor analysis. Several
studies have found between three and five such symptom dimensions: sym-metry/ordering, hoarding,
contamination/cleaning, aggressive obsessions/checking and sexual/religious obsessions. The
sym-metry dimension has been associated with comorbid tic disor-der; in one
study, patients who scored high on this dimension had a relative risk for
chronic tic disorder that was 8.5 times higher than those scoring low on this
factor (Leckman et al., 1997). It
appears that these symptom dimensions are stable over time, that is, although a
patient’s specific obsessions and com-pulsions may change over time, new
obsessions and compul-sions that develop are often within the same symptom
dimen-sion as the previous symptoms. A study using positron emission tomography
to evaluate neural correlates of these symptom di-mensions suggests that dysfunction
in separate regions of the brain (e.g., striatum and prefrontal cortex) may
mediate these factors (Rauch et al.,
1998).
Data were analyzed from a number of placebo-controlled serotonin reuptake inhibitor (SRI) treatment studies to assess whether symptom factors or dimensions were associated with treatment response. No clear pattern emerged except that patients with hoarding obsession had a significantly poorer response to SRIs. Whether these identified dimensions are associated with response to behavioral treatment, biological markers, or genetic transmission has yet to be investigated.
The following descriptions of some common obsessions and compulsions
illustrate the clinical presentation of these symptoms. In some cases a
particular symptom may belong to more than one “type” of obsessive or
compulsive grouping. Thus it is often up to the clinician to decide which
category to place a symptom so that it best describes the patient’s symptoms
overall; it may even be best to classify it in more than one category. For
instance, a patient who has concerns about cancer may have handwashing as a
compulsion related to her somatic obsession. If this is the only reason that
she washes her hands, to avoid get-ting cancer, you might simply classify this
as a somatic obsession with the accompanying compulsion. However if the patient
also washes repeatedly to avoid contamination in general, not just for cancer,
she would have both contamination and somatic obses-sions and compulsions.
Related Topics