Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hypertension
Nursing Process: The Patient With Hypertension
NURSING
PROCESS:THE PATIENT WITH HYPERTENSION
Assessment
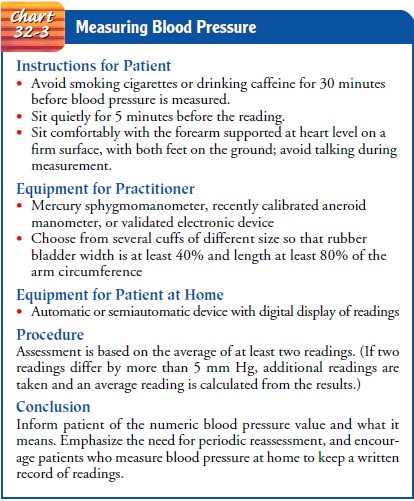
When hypertension is initially detected,
nursing assessment involves carefully monitoring the blood pressure at frequent
intervals and then, after diagnosis, at routinely scheduled intervals. The
Ameri-can Heart Association and the American Society of Hypertension have
defined the standards for blood pressure measurement, in cluding conditions
required before measurements are made, equip-ment specifications, and techniques
for measuring blood pressure to obtain accurate and reliable readings (Chart
32-3) (American Soci-ety of Hypertension, 1992; Perloff et al., 1993) When the
patient begins an antihypertensive treatment regimen, blood pressure
as-sessments are needed to determine the effectiveness of medication therapy
and to detect any changes in blood pressure that indicate the need for a change
in the treatment plan.
A
complete history is obtained to assess for symptoms that in-dicate target organ
damage (whether other body systems have been affected by the elevated blood
pressure). Such symptoms may in-clude anginal pain; shortness of breath;
alterations in speech, vision, or balance; nosebleeds; headaches; dizziness; or
nocturia.
During
the physical examination, the nurse must also pay specific attention to the
rate, rhythm, and character of the api-cal and peripheral pulses to detect
effects of hypertension on the heart and blood vessels. A thorough assessment
can yield valu-able information about the extent to which the hypertension has
affected the body and about any other personal, social, or financial factors
related to the condition.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, nursing diagnoses for the patient may include the
following:
· Deficient knowledge
regarding the relation between the treatment regimen and control of the disease
process
·
Noncompliance with therapeutic regimen related to
side effects of prescribed therapy
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications that may develop
include the following:
· Left ventricular
hypertrophy
· Myocardial infarction
· Heart failure
· TIAs
·
Cerebrovascular accident (stroke or brain attack)
•
Renal insufficiency and failure
•
Retinal hemorrhage
Planning and Goals
The major goals for the patient include understanding of the dis-ease process and its treatment, participation in a self-care pro-gram, and absence of complications.
Nursing Interventions
The
objective of nursing care for hypertensive patients focuses on lowering and
controlling the blood pressure without adverse effects and without undue cost.
To achieve these goals, the nurse must support and teach the patient to adhere
to the treatment regimen by implementing necessary lifestyle changes, taking
medications as prescribed, and scheduling regular follow-up appointments with
the health care provider to monitor progress or identify and treat any
complications of disease or therapy.
INCREASING KNOWLEDGE
The patient needs to understand the disease process and how lifestyle changes and medications can control hypertension. The nurse needs to emphasize the concept of controlling hypertension rather than curing it. The nurse can encourage the patient to con-sult a dietitian to help develop a plan for weight loss. The program usually consists of restricting sodium and fat intake, increasing intake of fruits and vegetables, and implementing regular physical activity. Explaining that it takes 2 to 3 months for the taste buds to adapt to changes in salt intake may help the patient adjust to re-duced salt intake.
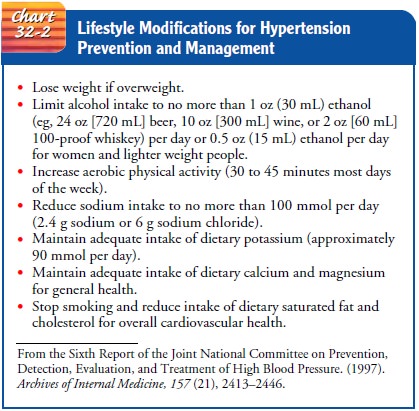
The patient should be advised to limit alcohol intake
(see Chart 32-2 for specific recommendations), and tobacco should be
avoided—not because smoking is related to hyper-tension, but because anyone
with high blood pressure is already at increased risk for heart disease, and
smoking amplifies this risk. Support groups for weight control, smoking
cessation, and stress reduction may be beneficial for some patients; others can
benefit from the support of family and friends. The nurse assists the pa-tient
to develop and adhere to an appropriate exercise regimen, because regular
activity is a significant factor in weight reduction and a blood pressure–reducing
intervention in the absence of any loss in weight (Sixth Report of the Joint
National Committee on Prevention, Detection, Evaluation, and Treatment of High
Blood Pressure, 1997).
PROMOTING HOME AND COMMUNITY-BASED CARE
Blood
pressure screenings with the sole purpose of case finding are not recommended
by the National High Blood Pressure Education Program because approximately 70%
of persons with hypertension are already aware of their blood pressure levels
(JNC VI, 1997). If asked to participate in a blood pressure screening, the
nurse should be sure that proper blood pressure measurement tech-nique is being
used (see Chart 32-3), that the manometers used are calibrated (Perloff et al.,
1993), and that provision has been made to provide follow-up for any person
identified as having an elevated blood pressure. Adequate time should also be
allowed to teach people what the blood pressure numbers mean. Each person
should be given a written record of his or her blood pressure at the screening.
Teaching Patients Self-Care
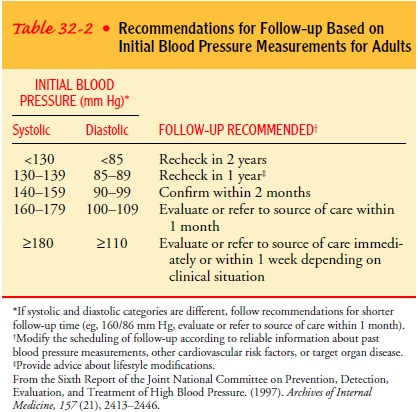
The
therapeutic regimen is the responsibility of the patient in collaboration with
the health care provider. Education about high blood pressure and how to manage
it, including medica-tions, lifestyle changes of diet, weight control, and
exercise (see Table 32-2), setting goal blood pressures, and assistance with
social support, can help the patient achieve blood pressure con-trol. Involving
family members in education programs enables them to support the patient’s
efforts to control hypertension. The American Heart Association and the
National Heart Lung and Blood Institute provide printed and electronic patient
education materials.
Written
information about the expected effects and side effects of medications is
important. When side effects occur, patients need to understand the importance
of reporting them and to whom they should be reported. Patients need to be
informed that reboundhypertension can
occur if antihypertensive medications are sud-denly stopped. Female and male
patients should be informed that some medications, such as beta-blockers, may
cause sexual dys-function and that, if a problem with sexual function or
satisfaction occurs, other medications are available. The nurse can encourage
and teach patients to measure their blood pressure at home. This practice
involves patients in their own care and emphasizes the fact that failing to
take medications may result in an identifiable rise in blood pressure. Patients
need to know that blood pressure varies continuously and that the range within
which their pressure varies should be monitored.
Continuing Care
Regular
follow-up care is imperative so that the disease process can be assessed and
treated, depending on whether control or progression is found. A history and
physical examination should be completed at each clinic visit. The history
should include all data that pertain to any potential problem, specifically
medication-related problems such as postural (orthostatic) hypotension
(experienced as dizziness or lightheadedness).
Deviation
from the therapeutic program is a significant prob-lem for people with
hypertension and other chronic conditions requiring lifetime management. It is
estimated that 50% dis-continue their medications within 1 year of beginning to
take them. Blood pressure control is achieved by only 27% (JNC VI, 1997).
However, when patients actively participate in self-care, including
self-monitoring of blood pressure and diet, compliance increases— possibly
because patients receive immediate feedback and have a greater sense of
control.
Considerable
effort is required by patients with hypertension to adhere to recommended
lifestyle modifications and to take reg-ularly prescribed medications. The
effort needed to follow the therapeutic plan may seem unreasonable to some,
particularly when they have no symptoms without medications but do have side
effects with medications. The recommended lifestyle changes are listed in Chart
32-2. Continued education and encourage-ment are usually needed to enable
patients to formulate an ac-ceptable plan that helps them live with their
hypertension and adhere to the treatment plan. Compromises may have to be made
about some aspects of therapy to achieve success in higher-priority goals. The
nurse can assist with behavior change by supporting patients in making small
changes with each visit that move them toward their goals. Another important
factor is following up at each visit to see how the patient has progressed with
the plansmade at the prior visit. If the patient has had difficulty with a
par-ticular aspect of the plan, the patient and nurse can work together to
develop an alternative or modification to the plan that the patient believes
will be more successful.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Symptoms suggesting that hypertension is
progressing to the extent that target organ damage is occurring must be
detected early so that appropriate treatment can be initiated accordingly. When
the pa-tient returns for follow-up care, all body systems must be assessed to
detect any evidence of vascular damage. Examining the eyes with an
ophthalmoscope is particularly important because retinal blood ves-sel damage
indicates similar damage elsewhere in the vascular sys-tem. The patient is
questioned about blurred vision, spots in front of the eyes, and diminished
visual acuity. The heart, nervous system, and kidneys are also carefully
assessed and examined. Any signifi-cant findings are promptly reported to
determine whether addi-tional diagnostic studies are required. Based on the
findings, medications may be changed to improve blood pressure control.
Gerontologic Considerations
Compliance
with the therapeutic program may be more difficult for elderly people. The
medication regimen can be difficult to remember, and the expense can be a
problem. Monotherapy (treatment with
a single agent), if appropriate, may simplify the medication regimen and make
it less expensive. Special care must be taken to ensure that the elderly
patient understands the regi-men and can see and read instructions, open the
medication con-tainer, and get the prescription refilled. The elderly person’s
family or caregivers should be included in the teaching program so that they
can understand the patient’s needs, encourage ad-herence to the treatment plan,
and know when and whom to call if problems arise or information is needed.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Maintains adequate
tissue perfusion
a) Maintains blood pressure
at less than 140/90 mm Hg (or less than 130/85 mm Hg for persons with diabetes
mellitus or proteinuria greater than 1 g per 24 hours) with lifestyle
modifications, medications, or both
b) Demonstrates no symptoms
of angina, palpitations, or vision changes
c) Has stable BUN and serum
creatinine levels
d) Has palpable peripheral
pulses
2) Complies with the
self-care program
a) Adheres to the dietary
regimen as prescribed: reduces calo-rie, sodium, and fat intake; increases
fruit and vegetable intake
b)
Exercises regularly
c)
Takes medications as prescribed and reports any
side effects
d)
Measures blood pressure routinely
e)
Abstains from tobacco and excessive alcohol intake
f)
Keeps follow-up appointments
3) Has no complications
a)
Reports no changes in vision
b)
Exhibits no retinal damage on vision testing
c) Maintains pulse rate and
rhythm and respiratory rate within normal ranges
d)
Reports no dyspnea or edema
e)
Maintains urine output consistent with intake
f)
Has renal function test results within normal range
g)
Demonstrates no motor, speech, or sensory deficits
h)
Reports no headaches, dizziness, weakness, changes
in gait, or falls
Related Topics