Chapter: Medical Surgical Nursing: Management of Patients With Cerebrovascular Disorders
Nursing Process: The Patient Recovering from an Ischemic Stroke
NURSING PROCESS: THE PATIENT
RECOVERING FROM AN ISCHEMIC STROKE
The
acute phase of an ischemic stroke may last 1 to 3 days, but ongoing monitoring
of all body systems is essential as long as the patient requires care. The
patient who has had a stroke is at risk for multiple complications, including
deconditioning and other musculoskeletal problems, swallowing difficulties,
bowel and blad-der dysfunction, inability to perform self-care, and skin
break-down. After the stroke is complete, management focuses on the prompt
initiation of rehabilitation for any deficits.
Assessment
During
the acute phase, a neurologic flow sheet is maintained to provide data about
the following important measures of the patient’s clinical status:
·
Change in the level of
consciousness or responsiveness as ev-idenced by movement, resistance to
changes of position, and response to stimulation; orientation to time, place,
and person
·
Presence or absence of
voluntary or involuntary movements of the extremities; muscle tone; body
posture; and position of the head
·
Stiffness or flaccidity of the
neck
·
Eye opening, comparative size
of pupils and pupillary reac-tions to light, and ocular position
·
Color of the face and
extremities; temperature and moisture of the skin
·
Quality and rates of pulse and
respiration; arterial blood gas values as indicated, body temperature, and
arterial pressure
·
Ability to speak
·
Volume of fluids ingested or
administered; volume of urine excreted each 24 hours
·
Presence of bleeding
·
Maintenance of blood pressure
within the desired param-eters
After the acute phase, the nurse assesses mental
status (memory, attention span, perception, orientation, affect,
speech/language), sensation/perception (usually the patient has decreased
aware-ness of pain and temperature), motor control (upper and lower extremity
movement), swallowing ability, nutritional and hydra-tion status, skin
integrity, activity tolerance, and bowel and blad-der function. Ongoing nursing
assessment continues to focus on any impairment of function in the patient’s
daily activities, because the quality of life after stroke is closely related
to the patient’s functional status.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses for a patient with a stroke
may include:
·
Impaired physical mobility
related to hemiparesis, loss of balance and coordination, spasticity, and brain
injury
·
Acute pain (painful shoulder)
related to hemiplegia and disuse
·
Self-care deficits (hygiene,
toileting, grooming, and feeding) related to stroke sequelae
·
Disturbed sensory perception
related to altered sensory re-ception, transmission, and/or integration
·
Impaired swallowing
·
Incontinence related to
flaccid bladder, detrusor instability, confusion, or difficulty in
communicating
·
Disturbed thought processes
related to brain damage, con-fusion, or inability to follow instructions
·
Impaired verbal communication
related to brain damage
·
Risk for impaired skin
integrity related to hemiparesis/ hemiplegia, or decreased mobility
·
Interrupted family processes
related to catastrophic illness and caregiving burdens
·
Sexual dysfunction related to
neurologic deficits or fear of failure
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Potential
complications include:
·
Decreased cerebral blood flow
due to increased ICP
·
Inadequate oxygen delivery to
the brain
·
Pneumonia
Planning and Goals
Although rehabilitation begins on the day the
patient has the stroke, the process is intensified during convalescence and
requires a coordinated team effort. It is helpful for the team to know whatthe
patient was like before the stroke: his or her illnesses, abilities, mental and
emotional state, behavioral characteristics, and activ-ities of daily living.
It is also helpful for clinicians to be knowl-edgeable about the relative
importance of predictors of stroke outcome (age, gender, NIHSS score at time of
admission, to name a few) in order to provide stroke survivors and their
families with realistic goals (Demchuk & Buchan, 2000).
The major goals for the patient (and family) may
include im-proved mobility, avoidance of shoulder pain, achievement of
self-care, relief of sensory and perceptual deprivation, prevention of
aspiration, continence of bowel and bladder, improved thought processes,
achieving a form of communication, maintaining skin integrity, restored family
functioning, improved sexual function, and absence of complications.
Nursing Interventions
Nursing care has a significant impact on the
patient’s recovery. Often many body systems are impaired as a result of the
stroke, and conscientious care and timely interventions can prevent
de-bilitating complications. During and after the acute phase, nurs-ing
interventions focus on the whole person. In addition to providing physical
care, nurses can encourage and foster recovery by listening to patients and
asking questions to elicit the mean-ing of the stroke experience (Eaves, 2000;
Pilkington, 1999).
IMPROVING MOBILITY AND PREVENTING JOINT DEFORMITIES
A
hemiplegic patient has unilateral paralysis (paralysis on one side). When
control of the voluntary muscles is lost, the strong flexor muscles exert
control over the extensors. The arm tends to adduct (adductor muscles are
stronger than abductors) and to ro-tate internally. The elbow and the wrist
tend to flex, the affected leg tends to rotate externally at the hip joint and
flex at the knee, and the foot at the ankle joint supinates and tends toward
plan-tar flexion.
Correct positioning is important to prevent
contractures; measures are used to relieve pressure, assist in maintaining good
body alignment, and prevent compressive neuropathies, especially of the ulnar
and peroneal nerves. Because flexor muscles are stronger than extensor muscles,
a posterior splint applied at night to the affected extremity may prevent
flexion and maintain correct po-sitioning during sleep.
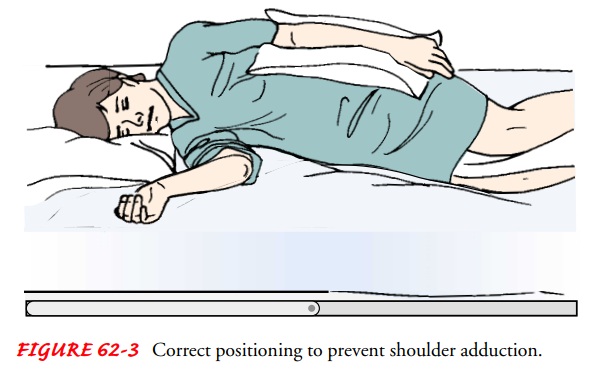
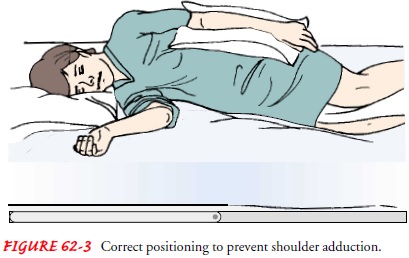
Preventing Shoulder Adduction
To
prevent adduction of the affected shoulder while the patient is in bed, a
pillow is placed in the axilla when there is limited ex-ternal rotation; this
keeps the arm away from the chest. A pillow is placed under the arm, and the
arm is placed in a neutral (slightly flexed) position, with distal joints
positioned higher than the more proximal joints. Thus, the elbow is positoned
higher than the shoulder and the wrist higher than the elbow. This helps to
prevent edema and the resultant joint fibrosis that will limit range of motion
if the patient regains control of the arm (Fig. 62-3).
Positioning the Hand and Fingers
The fingers are positioned so that they are barely flexed. The hand is placed in slight supination (palm faces upward), which is its most functional position. If the upper extremity is flaccid, a volar resting splint can be used to support the wrist and hand in a func-tional position. If the upper extremity is spastic, a hand roll is not used, because it stimulates the grasp reflex. In this instance a dorsal wrist splint is useful in allowing the palm to be free of pres-sure. Every effort is made to prevent hand edema.
Spasticity,
particularly in the hand, can be a disabling com-plication after stroke.
Researchers have recently reported that in-tramuscular injections of botulinum
toxin A decreased spasticity in the wrist and fingers and increased functional
ability in dress-ing, washing, and other activities of daily living (Brashear
et al., 2002).
Changing Positions
The
patient’s position should be changed every 2 hours. To place a patient in a
lateral (side-lying) position, a pillow is placed be-tween the legs before the
patient is turned. To promote venous return and prevent edema, the upper thigh
should not be acutely flexed. The patient may be turned from side to side, but
the amount of time spent on the affected side should be limited if sensation is
impaired.
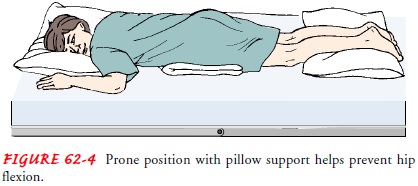
If
possible, the patient is placed in a prone position for 15 to 30 minutes
several times a day. A small pillow or a support is placed under the pelvis,
extending from the level of the umbili-cus to the upper third of the thigh
(Fig. 62-4). This helps to pro-mote hyperextension of the hip joints, which is
essential for normal gait and helps prevent knee and hip flexion contractures.
The prone position also helps to drain bronchial secretions and prevents
contractural deformities of the shoulders and knees. During positioning, it is
important to reduce pressure and change position frequently to prevent pressure
ulcers.
Establishing an Exercise Program
The affected extremities are exercised passively and put through a full range of motion four or five times a day to maintain joint mobility,
regain motor control, prevent contractures in the para-lyzed extremity, prevent
further deterioration of the neuro-muscular system, and enhance circulation.
Exercise is helpful in preventing venous stasis, which may predispose the
patient to thrombosis and pulmonary embolus.
Repetition
of an activity forms new pathways in the CNS and therefore encourages new
patterns of motion. At first, the ex-tremities are usually flaccid. If
tightness occurs in any area, the range-of-motion exercises should be performed
more frequently.
The
patient is observed for signs and symptoms that may in-dicate pulmonary embolus
or excessive cardiac workload during exercise; these include shortness of
breath, chest pain, cyanosis, and increasing pulse rate with exercise. Frequent
short periods of exercise always are preferable to longer periods at infrequent
in-tervals. Regularity in exercise is most important. Improvement in muscle
strength and maintenance of range of motion can be achieved only through daily
exercise.
The patient is encouraged and reminded to exercise
the un-affected side at intervals throughout the day. It is helpful to de-velop
a written schedule to remind the patient of the exercise activities. The nurse
supervises and supports the patient during these activities. The patient can be
taught to put the unaffected leg under the affected one to move it when turning
and exercis-ing. Flexibility, strengthening, coordination, endurance, and
bal-ancing exercises prepare the patient for ambulation. Quadriceps muscle
setting and gluteal setting exercises are started early to im-prove the muscle
strength needed for walking; these are per-formed at least five times daily for
10 minutes at a time.
Preparing for Ambulation
As
soon as possible, the patient is assisted out of bed. Usually, when hemiplegia
has resulted from a thrombosis, an active reha-bilitation program is started as
soon as the patient regains con-sciousness; a patient who has had a cerebral
hemorrhage cannot participate actively until all evidence of bleeding is gone.
The
patient is first taught to maintain balance while sitting and then to learn to
balance while standing. If the patient has dif-ficulty in achieving standing
balance, a tilt table, which slowly brings the patient to an upright position,
can be used. Tilt tables are especially helpful for patients who have been on
bed rest for prolonged periods and are having orthostatic blood pressure
changes.
If
the patient needs a wheelchair, the folding type with hand brakes is the most
practical because it allows the patient to ma-nipulate the chair. The chair
should be low enough to allow the patient to propel it with the uninvolved foot
and narrow enough to permit it to be used in the home. When the patient is
trans-ferred from the wheelchair, the brakes must be applied and locked on both
sides of the chair.
The
patient is usually ready to walk as soon as standing bal-ance is achieved.
Parallel bars are useful in these first efforts. A chair or wheelchair should
be readily available in case the patient suddenly becomes fatigued or feels
dizzy.
The training periods for ambulation should be short
and fre-quent. As the patient gains strength and confidence, an adjustable cane
can be used for support. Generally, a three- or four-pronged cane provides a
stable support in the early phases of rehabilitation.
PREVENTING SHOULDER PAIN
Up to 70% of stroke patients suffer severe pain in
the shoulder that prevents them from learning new skills, because shoulder
function is essential in achieving balance and performing transfers and
self-care activities. Three problems can occur: painful shoulder, subluxation
of the shoulder, and shoulder–hand syndrome.
A flaccid shoulder joint may be overstretched by
the use of ex-cessive force in turning the patient or from overstrenuous arm
and shoulder movement. To prevent shoulder pain, the nurse should never lift
the patient by the flaccid shoulder or pull on the affected arm or shoulder. If
the arm is paralyzed, subluxation (incomplete dislocation) at the shoulder can
occur from over-stretching the joint capsule and musculature by the force of
grav-ity when the patient sits or stands in the early stages after a stroke.
This results in severe pain. Shoulder–hand syndrome (painful shoulder and
generalized swelling of the hand) can cause a frozen shoulder and ultimately
atrophy of subcutaneous tissues. When a shoulder becomes stiff, it is usually
painful.
Medications are helpful in the management of
post-stroke pain. Amitriptyline hydrochloride (Elavil) has been used but it can
cause cognitive problems, has a sedating effect, and is not effective in all
patients. A recent study showed the efficacy of an antiseizure medication
lamotrigine (Lamictal) in treating post-stroke pain (Jensen et al., 2001).
Many shoulder problems can be prevented by proper
patient movement and positioning. The flaccid arm is positioned on a table or
with pillows while the patient is seated. Some clinicians advocate the use of a
properly worn sling when the patient first becomes ambulatory to prevent the
paralyzed upper extremity from dangling without support. Range-of-motion
exercises are important in preventing painful shoulder. Overstrenuous arm
movements are avoided. The patient is instructed to interlace the fingers,
place the palms together, and push the clasped hands slowly forward to bring
the scapulae forward; he or she then raises both hands above the head. This is
repeated throughout the day. The patient is instructed to flex the affected
wrist at intervals and move all the joints of the affected fingers. He or she
is encouraged to touch, stroke, rub, and look at both hands. Pushing the heel
of the hand firmly down on a surface is useful. Elevation of the arm and hand
is also important in preventing dependent edema of the hand. Patients with
continuing pain after movement and positioning have been attempted may require
the addition of analgesia to their treatment program.
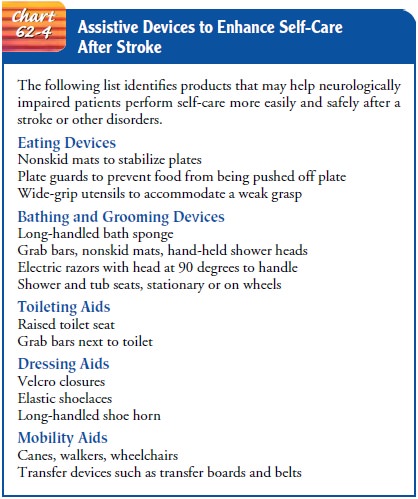
ENHANCING SELF-CARE
As soon as the patient can sit up, personal hygiene
activities are encouraged. The patient is helped to set realistic goals; if
feasible, a new task is added daily. The first step is to carry out all
self-care activities on the unaffected side. Such activities as combing the
hair, brushing the teeth, shaving with an electric razor, bathing, and eating
can be carried out with one hand and are suitable for self-care. Although the
patient may feel awkward at first, the var-ious motor skills can be learned by
repetition, and the unaffected side will become stronger with use. The nurse
must be sure that the patient does not neglect the affected side. Assistive
devices will help make up for some of the patient’s deficits (Chart 62-4). A
small towel is easier to control while drying after bathing, and boxed paper
tissues are easier to use than a roll of toilet tissue.
Return of functional ability is important to the patient recov-ering after a stroke. An early baseline assessment of functional ability with an instrument such as the Functional Independence Measure (FIM) is important in team planning and goal setting for the patient. The FIM is a widely used instrument in stroke re-habilitation and also provides valuable functional information during the acute phase of care (Hinkle, 2000, 2001).
The
patient’s morale will improve if ambulatory activities are carried out in
street clothes. The family is instructed to bring in clothing that is
preferably a size larger than that normally worn. Clothing fitted with front or
side fasteners or Velcro closures is the most suitable. The patient has better
balance if most of the dressing activities are done in a seated position.
Perceptual
problems may make it difficult for the patient to dress without assistance
because of an inability to match the clothing to the body parts. To assist the
patient, the nurse can take steps to keep the environment organized and
uncluttered, because the patient with a perceptual problem is easily
distracted. The clothing is placed on the affected side in the order in which
the garments are to be put on. Using a large mirror while dress-ing promotes
the patient’s awareness of what he or she is putting on the affected side. Each
garment is put on the affected side first. The patient has to make many
compensatory movements when dressing; these can produce fatigue and painful
twisting of the in-tercostal muscles. Support and encouragement are provided to
prevent the patient from becoming overly fatigued and discour-aged. Even with
intensive training, not all patients can achieve independence in dressing.
MANAGING SENSORY-PERCEPTUAL DIFFICULTIES
Patients
with a decreased field of vision should be approached on the side where visual
perception is intact. All visual stimuli (clock, calendar, and television)
should be placed on this side. The pa-tient can be taught to turn the head in
the direction of the defec-tive visual field to compensate for this loss. The
nurse should make eye contact with the patient and draw his or her attention to
the affected side by encouraging the patient to move the head. The nurse may
also want to stand at a position that encourages the patient to move or turn to
visualize who is in the room. Increasing the natural or artificial lighting in
the room and pro-viding eyeglasses are important in increasing vision.The
patient with homonymous hemianopsia (loss of half of the visual field) turns
away from the affected side of the body and tends to neglect that side and the
space on that side; this is called amorphosynthesis. In such instances, the
patient cannot see food on half of the tray, and only half of the room is
visible. It is im-portant for the nurse to constantly remind the patient of the
other side of the body, to maintain alignment of the extremities, and, if
possible, to place the extremities where the patient can see them.
MANAGING DYSPHAGIA
Stroke
can result in swallowing problems (dysphagia) due to im-paired function of the
mouth, tongue, palate, larynx, pharynx, or upper esophagus. Patients must be
observed for paroxysms of coughing, food dribbling out of or pooling in one
side of the mouth, food retained for long periods in the mouth, or nasal re-gurgitation
when swallowing liquids. Swallowing difficulties place the patient at risk for
aspiration, pneumonia, dehydration, and malnutrition.
A speech therapist will evaluate the patient’s gag
reflexes and ability to swallow. Even if partially impaired, swallowing
func-tion may return in some patients over time, or the patient may be taught
alternative swallowing techniques, advised to take smaller boluses of food, and
taught about which foods are easier to swal-low. The patient may initially be
started on a thick liquid or puréed diet because these foods are easier to
swallow than thin liquids. Having the patient sit upright, preferably out of
bed in a chair, and instructing him or her to tuck the chin toward the chest as
he or she swallows, will help prevent aspiration. The diet may be advanced as
the patient becomes more proficient at swal-lowing. If the patient cannot
resume oral intake, a gastrointesti-nal feeding tube will be placed for ongoing
tube feedings.
Managing Tube Feedings
Enteral tubes can be either nasogastric (placed in
the stomach) or nasoenteral (placed in the duodenum) to reduce the risk of
aspi-ration. Nursing responsibilities in feeding include elevating the head of
the bed at least 30 degrees to prevent aspiration, check-ing the position of
the tube before feeding, ensuring that the cuff of the tracheostomy tube (if in
place) is inflated, and giving the tube feeding slowly. The feeding tube is
aspirated periodically to ensure that the feedings are passing through the
gastrointestinal tract. Retained or residual feedings increase the risk for
aspiration. Patients with retained feedings may benefit from the placement of a
gastrostomy tube or a percutaneous endoscopic gastrostomy tube. In a patient
with a nasogastric tube, the feeding tube should be placed in the duodenum to
reduce the risk of aspiration. For long-term feedings, a gastrostomy tube is
preferred.
ATTAINING BOWEL AND BLADDER CONTROL
After a stroke, the patient may have transient
urinary inconti-nence due to confusion, inability to communicate needs, and
in-ability to use the urinal or bedpan because of impaired motor and postural
control. Occasionally after a stroke, the bladder becomes atonic, with impaired
sensation in response to bladder filling. Sometimes control of the external
urinary sphincter is lost or di-minished. During this period, intermittent
catheterization with sterile technique is carried out. When muscle tone
increases and deep tendon reflexes return, bladder tone increases and
spasticity of the bladder may develop. Because the patient’s sense of
aware-ness is clouded, persistent urinary incontinence or urinary reten-tion
may be symptomatic of bilateral brain damage. The voiding pattern is analyzed
and the urinal or bedpan offered on this pat-tern or schedule. The upright
posture and standing position are helpful for male patients during this aspect
of rehabilitation.
Patients
may also have problems with bowel control or con-stipation, with constipation
being more common. Unless con-traindicated, a high-fiber diet and adequate
fluid intake (2 to 3 L per day) should be provided and a regular time
established (usu-ally after breakfast) for toileting.
IMPROVING THOUGHT PROCESSES
After
a stroke, the patient may have problems with cognitive, be-havioral, and emotional
deficits related to brain damage. In many instances, however, a considerable
degree of function can be re-covered because not all areas of the brain are
equally damaged; some remain more intact and functional than others.
After
assessment that delineates the patient’s deficits, the neu-ropsychologist, in
collaboration with the primary care physician, psychiatrist, nurse, and other
professionals, structures a training program using cognitive-perceptual
retraining, visual imagery, reality orientation, and cueing procedures to
compensate for losses.
The
role of the nurse is supportive. The nurse reviews the results of
neuropsychological testing, observes the patient’s per-formance and progress,
gives positive feedback, and, most impor-tantly, conveys an attitude of
confidence and hope. Interventions capitalize on the patient’s strengths and
remaining abilities while attempting to improve performance of affected
functions. Other interventions are similar to those for improving cognitive
func-tioning after a head injury.
IMPROVING COMMUNICATION
Aphasia,
which impairs the patient’s ability to understand what is being said and to
express himself or herself, may become ap-parent in various ways. The cortical
area responsible for integrat-ing the myriad of pathways required for the
comprehension and formulation of language is called Broca’s area. It is located
in a convolution adjoining the middle cerebral artery. This area is
re-sponsible for control of the combinations of muscular move-ments needed to
speak each word. Broca’s area is so close to the left motor area that a
disturbance in the motor area often affects the speech area. This is why so
many patients paralyzed on the right side (due to damage or injury to the left
side of the brain) cannot speak, whereas those paralyzed on the left side are
less likely to have speech disturbances.
The
speech pathologist assesses the communication needs of the stroke patient,
describes the precise deficit, and suggests the best overall method of
communication. With many language in-tervention strategies for the aphasic
adult, the program can be in-dividually tailored. The patient is expected to
take an active part in establishing goals.
A
person with aphasia may become depressed because of the inability to talk. The
inability to talk on the telephone, answer a question, or participate in
conversation causes anger, frustration, fear of the future, and hopelessness.
Nursing interventions in-clude doing everything possible to make the atmosphere
con-ducive to communication. This includes being sensitive to the patient’s
reactions and needs and responding to them in an ap-propriate manner, always
treating the patient as an adult. The nurse provides strong moral support and
understanding to allay anxiety.
A
common pitfall is for the nurse or other health care team member to complete
the thoughts or sentences of the patient.This should be avoided because it may
cause the patient to feel more frustrated at not being allowed to speak and may
deter ef-forts to practice putting thoughts together and completing the
sentence. A consistent schedule, routines, and repetitions help the patient to
function despite significant deficits. A written copy of the daily schedule, a
folder of personal information (birth date, address, names of relatives),
checklists, and an audiotaped list help improve the patient’s memory and
concentration. The pa-tient may also benefit from a communication board, which
has pictures of common needs and phrases. The board may be trans-lated into
several languages.
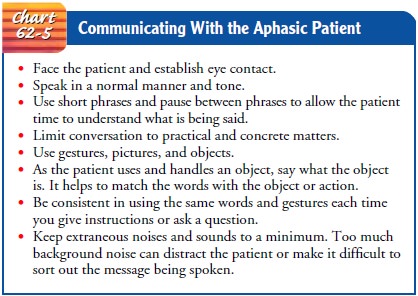
When
talking with the patient, it is important to have the pa-tient’s attention,
speak slowly, and keep the language of instruc-tion consistent. One instruction
is given at a time, and time is allowed for the patient to process what has
been said. The use of gestures may enhance comprehension. Speaking is thinking
out loud, and the emphasis is on thinking. The patient must sort out incoming
messages and formulate a response. Listening requires mental effort; the
patient must struggle against mental inertia and needs time to organize an
answer.
In
working with the aphasic patient, the nurse must remem-ber to talk to the
patient during care activities. This provides so-cial contact for the patient.
Chart 62-5 describes points to keep in mind when communicating with the aphasic
patient.
MAINTAINING SKIN INTEGRITY
The stroke patient may be at risk for skin and
tissue breakdown because of altered sensation and inability to respond to
pressure and discomfort by turning and moving. Therefore, preventing skin and
tissue breakdown requires frequent assessment of the skin, with emphasis on
bony areas and dependent parts of the body. During the acute phase, a specialty
bed (eg, low-air-loss bed) may be used until the patient can move independently
or as-sist in moving.
A regular turning and positioning schedule must be followed to minimize pressure and prevent skin breakdown. Pressure-relieving devices may be employed but do not replace regular turn-ing and positioning. The turning schedule (at least every 2 hours) must be adhered to even if pressure-relieving devices are used to prevent tissue and skin breakdown. When the patient is posi-tioned or turned, care must be used to minimize shear and friction forces, which cause damage to tissues and predispose the skin to breakdown.
The patient’s skin must be kept clean and dry;
gentle massage of healthy (nonreddened) skin and adequate nutrition are other
factors that help to maintain normal skin and tissue integrity.
IMPROVING FAMILY COPING
Family
members play an important role in the patient’s recovery. Some type of
counseling and support system should be available to them to prevent the care
of the patient from taking a signifi-cant toll on their health and interfering
too radically with their lives. Involving others in the patient’s care and
teaching stress management techniques and methods for maintaining personal
health also facilitate family coping.
The
family may have difficulty accepting the patient’s disabil-ity and may be
unrealistic in their expectations. They are given information about the
expected outcomes and are counseled to avoid doing for the patient those things
that he or she can do. They are assured that their love and interest are part
of the pa-tient’s therapy.
The
family needs to be informed that the rehabilitation of the hemiplegic patient
requires many months; progress may be slow. The gains made by the patient in
the hospital or rehabilitation unit must be maintained. All should approach the
patient with a supportive and optimistic attitude, focusing on the abilities
that remain. The rehabilitation team, the medical and nursing team, the
patient, and the family all must be involved in developing at-tainable goals
for the patient at home.
Most
relatives of stroke patients handle the physical changes better than the
emotional aspects of care. The family should be prepared to expect occasional
episodes of emotional lability. The patient may laugh or cry easily and may be
irritable and de-manding or depressed and confused. The nurse can explain to
the family that the patient’s laughter does not necessarily connote happiness,
nor does crying reflect sadness, and that emotional la-bility usually improves
with time.
HELPING THE PATIENT COPE WITH SEXUAL DYSFUNCTION
Sexual functioning can be profoundly altered by
stroke. Often stroke is such a catastrophic illness that the patient
experiences loss of self-esteem and value as a sexual being. Although research
in this area of stroke management is limited, it appears that stroke patients
consider sexual function to be important, but most have sexual dysfunction. The
combined effects of age and stroke cause a marked decline in many aspects of
sexuality (Lipski & Alexan-der, 1997). In-depth assessments to determine sexual
history be-fore and after the stroke should be followed by appropriate
interventions. Interventions for the patient and partner focus on providing
relevant information, education, reassurance, adjust-ment of medications,
counseling regarding coping skills, sugges-tions for alternative positions, and
a means of sexual expression and satisfaction (Lipski & Alexander, 1997).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patient and family education is a fundamental
component of re-habilitation, and ample opportunity for learning about stroke,
its causes and prevention, and the rehabilitation process should be provided
(Mumma, 2001). In both acute care and rehabilitation facilities, the focus is
on teaching patients to resume as much self-care as possible. This may entail
using assistive devices or modifying the home environment to help the patient
live with a disability.
An
occupational therapist may be helpful in assessing the home environment and
recommending modifications to help the patient become more independent. For
example, a shower is more convenient than a tub for the hemiplegic patient
because most patients do not gain sufficient strength to get up and down from a
tub. Sitting on a stool of medium height with rubber suc-tion tips permits the
patient to wash with greater ease. A long-handled bath brush with a soap
container is helpful to the patient who has only one functional hand. If a
shower is not available, a stool may be placed in the tub and a portable shower
hose at-tached to the faucet. Handrails may be attached beside the bath-tub and
the toilet. Other assistive devices include special utensils for eating,
grooming, and dressing (see Chart 62-3).
Continuing Care
The
recovery and rehabilitation process after stroke may be pro-longed, requiring
patience and perseverance on the part of the pa-tient and family. Depending on
the specific neurologic deficits resulting from the stroke, the patient at home
may require the ser-vices of a number of health care professionals. The nurse
often coordinates the care of the patient at home. The family (often the
spouse) will require assistance in planning and providing care. The caregiver
often requires reminders to attend to his or her health problems and
well-being.
The
family is advised that the patient may tire easily, become irritable and upset
by small events, and is likely to show less in-terest in things. Because a
stroke frequently occurs in the later stages of life, there is the possibility
of intellectual decline related to dementia.
Emotional
problems associated with stroke are often related to speech dysfunction and
frustrations about being unable to communicate. A speech therapist who visits
the home allows the family to be involved and gives the family practical
instructions to help the patient between therapy sessions.
Depression is a common and serious problem in the
stroke pa-tient. Antidepressant therapy may help if depression dominates the
patient’s life. As progress is made in the rehabilitation program, some
problems will diminish. The family can help by continuing to support the
patient and by giving positive reinforcement for the progress that is being
made.
Community-based stroke support groups allow the
patient and family to learn from others with similar problems and to share
their experiences (Olson, 2001). The patient is encouraged to continue with
hobbies, recreational and leisure interests, and contact with friends to
prevent social isolation. All nurses com-ing in contact with the patient should
encourage the patient to keep active, adhere to the exercise program, and
remain as self-sufficient as possible.
The nurse should recognize the potential effects of
caregiving on the family (Teel et al., 2001). Not all families have the
adap-tive coping skills and psychological functioning necessary for the
long-term care of another. The patient’s spouse may be elderly, with his or her
own health problems; in some instances the stroke patient may have been the
provider of care to the spouse. Even healthy caregivers may find it difficult
to maintain a schedule that includes being available around the clock. Some
effects of sus-tained caregiving include increased risk for depression and
sub-stance abuse, and increased use of health care services by the caregiver
(King et al., 2001). Depressed caregivers are more likely to resort to physical
or emotional abuse of the patient and are more likely to place the patient in a
nursing home. Respite care(planned short-term care to relieve the family from
having to pro-vide continuous 24-hour care) may be available from an adult day
care center. Some hospitals also offer weekend respite care that can provide
caregivers with needed time to themselves. Nurses should encourage families to
arrange for such services and should provide information to assist them.
The nurse involved in home and continuing care also needs to remind patients and family members of the need for continuing health promotion and screening practices. Patients who have not been involved in these practices in the past are educated about their importance and are referred to appropriate health care providers, if indicated.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Achieves
improved mobility
a) Avoids
deformities (contractures and footdrop)
b) Participates
in prescribed exercise program
c) Achieves
sitting balance
d) Uses
unaffected side to compensate for loss of function of hemiplegic side
2) Reports
absence of shoulder pain
a) Demonstrates
shoulder mobility; exercises shoulder
b) Elevates
arm and hand at intervals
3) Achieves
self-care; performs hygiene care; uses adaptive equipment
4) Turns
head to see people or objects
5) Demonstrates
improved swallowing ability
6) Achieves
normal bowel and bladder elimination
7) Participates
in cognitive improvement program
8) Demonstrates
improved communication
9) Maintains
intact skin without breakdown
a) Demonstrates
normal skin turgor
b) Participates
in turning and positioning activities
10) Family
members demonstrate a positive attitude and cop-ing mechanisms
a) Encourage
patient in exercise program
b) Take
an active part in rehabilitation process
c) Contact
respite care programs or arrange for other fam-ily members to assume some
responsibilities for care
11) Has
positive attitude regarding alternative approaches to sexual expression
Related Topics