Chapter: Medical Surgical Nursing: Postoperative Nursing Management
Nursing Process: The Hospitalized Patient Recovering From Surgery
NURSING PROCESS: THE HOSPITALIZED PATIENT RECOVERING FROM
SURGERY
The
Perioperative Nursing Data Set (PNDS) is a helpful model used by nurses in the
postoperative phase of care. Phenomena of concern to nurses on the clinical
unit in the postoperative phase of care include nursing diagnoses,
in-terventions, and outcomes for patients and their families. Addi-tional areas
of concern include collaborative problems and expected goals.
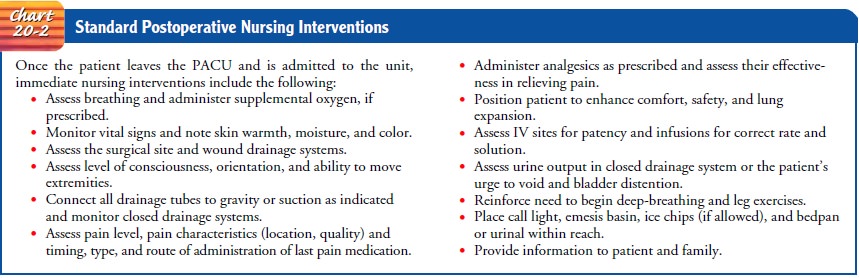
Assessment
Assessment
of the hospitalized postoperative patient includes monitoring vital signs and
completing a review of the systems upon arrival of the patient to the clinical
unit and thereafter (see Chart 20-2).
Respiratory
status is important because pulmonary complica-tions are among the most
frequent and serious problems encoun-tered by the surgical patient. The nurse
observes for airway patency and the quality of respirations, including depth,
rate, and sound. Chest auscultation verifies that breath sounds are normal (or
not normal) bilaterally, and the findings are documented as a baseline for
later comparisons. Often, because of the effects of pain medica-tions,
respirations are slow. Shallow and rapid respirations may be due to pain,
constricting dressings, gastric dilation, or obesity. Noisy breathing may be
due to obstruction by secretions or the tongue.
The
nurse assesses the patient’s pain level using a verbal or vi-sual analog scale
and assesses the characteristics of the pain. The patient’s appearance, pulse,
respirations, blood pressure, skin color (adequate or cyanotic), and skin
temperature (cold and clammy, warm and moist, or warm and dry) are clues to
cardiovascular func-tion. When the patient arrives in the clinical unit, the
surgical site is observed for bleeding, type and integrity of dressing, and
drains.
Also
assessed when the patient arrives on the clinical unit are the patient’s mental
status and level of consciousness, speech, and orientation in comparison with
preoperative baseline measures. Although a change in mental status or
postoperative restlessness may be related to anxiety, pain, or medications, it
may also be a symptom of oxygen deficit or hemorrhage. These serious causes
must be investigated and excluded before other causes are pursued.
General discomfort resulting from lying
in one position on the operating table, the surgeon’s handling of tissues, the
body’s reac-tion to anesthesia, and anxiety are also common causes of
restless-ness. These discomforts may be relieved by administering the
prescribed analgesics, changing the patient’s position frequently, and
assessing and alleviating the cause of anxiety. If tight, drainage-soaked
bandages are causing discomfort, reinforcing or changing the dressing
completely makes the patient more comfortable. The bladder is palpated for
distention because urinary retention can also cause restlessness.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, major nursing diagnoses may in-clude the following:
• Risk for ineffective airway clearance related to depressed res-piratory function, pain, and bed rest
• Acute pain related to surgical incision
• Decreased cardiac output related to shock or hemorrhage
• Activity intolerance related to generalized weakness sec-ondary to surgery
• Impaired skin integrity related to surgical incision and drains
• Risk for imbalanced body temperature related to surgical environment and anesthetic agents
• Risk for imbalanced nutrition, less than body requirements related to decreased intake and increased need for nutrients secondary to surgery
• Risk for constipation related to effects of medications, surgery, dietary change, and immobility
• Risk for urinary retention related to anesthetic agents
• Risk for injury related to surgical procedure or anesthetic agents
• Anxiety related to surgical procedure
• Risk for ineffective management of therapeutic regimen related to insufficient knowledge about wound care, di-etary restrictions, activity recommendations, medications, follow-up care, or signs and symptoms of complications
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications may in-clude the following:
• Deep vein thrombosis
• Hematoma
• Infection
• Wound dehiscence or evisceration
Planning and Goals
The
major goals for the patient include optimal respiratory func-tion, relief of
pain, optimal cardiovascular function, increased ac-tivity tolerance,
unimpaired wound healing, maintenance of body temperature, and maintenance of
nutritional balance. Fur-ther goals include resumption of usual pattern of
bowel and blad-der elimination, identification of any perioperative positioning
injury, acquisition of sufficient knowledge to manage self-care after
discharge, and absence of complications.
Nursing Interventions
PREVENTING RESPIRATORY COMPLICATIONS
Respiratory
depressive effects of opioid medications, decreased lung expansion secondary to
pain, and decreased mobility com-bine to put the patient at risk for common
respiratory complica-tions, particularly atelectasis (incomplete expansion of
the lung), pneumonia, and hypoxemia (Finkelmeier, 2000; Meeker & Rothrock,
1999). Atelectasis remains a risk for the patient who is not moving well or
ambulating or who is not performing deep-breathing and coughing exercises or
using an incentive spirome-ter. Signs and symptoms include decreased breath
sounds over the affected area, crackles, and cough. Pneumonia is character-ized
by chills and fever, tachycardia, and tachypnea. Cough may or may not be
present and may or may not be productive. Hypo-static pulmonary congestion,
caused by a weakened cardiovascular system that permits stagnation of
secretions at lung bases, may develop; it occurs most frequently in elderly
patients who are not mobilized effectively. The symptoms are often vague, with
per-haps a slight elevation of temperature, pulse, and respiratory rate and a
cough. Physical examination reveals dullness and crackles at the base of the
lungs. If the condition progresses, the outcome may be fatal.
The
types of hypoxemia that can affect postoperative patients are subacute and
episodic. Subacute hypoxemia is a constant low level of oxygen saturation,
although breathing appears normal. Episodic hypoxemia develops suddenly, and
the patient may be at risk for cerebral dysfunction, myocardial ischemia, and
cardiac arrest. Patients at risk for hypoxemia include those who have undergone
major surgery (particularly abdominal), are obese, or have preexisting
pulmonary problems. Hypoxemia can be de-tected by pulse oximetry, which
measures blood oxygen satura-tion. Factors that may affect the accuracy of
pulse oximetry readings include cold extremities, tremors, atrial fibrillation,
acrylic nails, and black or blue nail polish (these colors interfere with the
functioning of the pulse oximeter; other colors do not).
Preventive
measures and timely recognition of signs and symptoms help avert pulmonary
complications. Strategies to prevent respiratory complications include use of
an incentive spirometer and deep-breathing and coughing exercises. Crackles
indicate static pulmonary secretions that need to be mobilized by coughing and
deep-breathing exercises. When a mucus plug ob-structs one of the bronchi
entirely, the pulmonary tissue beyond the plug collapses, and a massive
atelectasis results.
To
clear secretions and prevent pneumonia, the nurse en-courages the patient to
turn frequently and take deep breaths at least every 2 hours. Coughing is also
encouraged to dislodge mucus plugs. These pulmonary exercises should begin as
soon as the patient arrives on the clinical unit and continue until the patient
is discharged. Even if he or she is not fully awake from anesthesia, the
patient can be asked to take several deep breaths. This helps to expel residual
anesthetic agents, mobilize secretions, and prevent alveolar collapse
(atelectasis). Careful splinting of ab-dominal or thoracic incision sites helps
the patient overcome the fear that the exertion of coughing might open the
incision. Anal-gesic agents are administered to permit more effective coughing,
and oxygen is administered as prescribed to prevent or relieve hypoxia. To
encourage lung expansion, the patient is encouraged to yawn or take sustained maximal
inspirations to create a nega-tive intrathoracic pressure of −40 mm Hg and expand lung volume to total capacity. Chest
physical therapy may be prescribed if indicated.
Coughing
is contraindicated in patients who have head in-juries or who have undergone
intracranial surgery (because of the risk for increasing intracranial
pressure), as well as in patients who have undergone eye surgery (risk for
increasing intraocular pres-sure) or plastic surgery (risk for increasing
tension on delicate tis-sues). In patients with an abdominal or thoracic
incision, the nurse teaches the patient how to splint the incision while
coughing.
Most
postoperative patients, especially the elderly and those with an abdominal or
thoracic incision, are given an incentive spirometer to use. In incentive
spirometry, the patient performs sustained maximal inspirations and can see the
results of these ef-forts as they register on the spirometer. Such feedback
encourages the patient to continue to take deep breaths to maximize volun-tary
lung expansion. A target is established for each patient. The patient first
exhales, then places the lips around the mouthpiece and slowly inhales, trying
to drive the piston on the device to a marked goal. Using a spirometer has
several advantages: it en-courages the patient to participate actively in
treatment; it ensures that the maneuver is physiologically appropriate and is
repeated; and it is a cost-effective way of preventing complications. A com-mon
recommendation for use of the incentive spirometer is 10 deep breaths every
hour while awake.
Early
ambulation increases metabolism and pulmonary aera-tion and, in general,
improves all body functions. The patient is encouraged to be out of bed as soon
as possible (ie, on the day of surgery, or no later than the first
postoperative day). This prac-tice is especially valuable in preventing
pulmonary complications in older patients.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
a.
Maintains optimal respiratory
function
i.
Performs deep-breathing exercises
ii.
Displays clear breath sounds
iii.
Uses incentive spirometer as
prescribed
iv.
Splints incisional site when coughing to
reduce pain
b.
Indicates that pain is decreased in
intensity
c.
Exercises and ambulates as
prescribed
i.
Alternates periods of rest and
activity
ii.
Progressively increases ambulation
iii.
Resumes normal activities within
prescribed time frame
iv.
Performs activities related to
self-care
d.
Wound heals without complication
e.
Maintains body temperature within
normal limits
f.
Resumes oral intake
i.
Reports absence of nausea and
vomiting
ii.
Takes at least 75% of usual diet
iii.
Is free of abdominal distress and
gas pains
iv.
Exhibits normal bowel sounds
g.
Reports resumption of usual bowel
elimination pattern
h.
Resumes usual voiding pattern
i.
Is free of injury
j.
Exhibits decreased anxiety
k.
Acquires knowledge and skills
necessary to manage ther-apeutic regimen
l.
Experiences no complications
Related Topics