Chapter: Medical Surgical Nursing: Postoperative Nursing Management
Nursing Management in the PACU
NURSING MANAGEMENT IN THE PACU
The
nursing management objectives for the patient in the PACU are to provide care
until the patient has recovered from the effects of anesthesia (eg, until
resumption of motor and sensory functions), is oriented, has stable vital
signs, and shows no evidence of hem-orrhage or other complications.
Assessing the Patient
Frequent,
skilled assessments of the blood oxygen saturation level, pulse rate and
regularity, depth and nature of respirations, skin color, level of
consciousness, and ability to respond to com-mands are the cornerstones of
nursing care in the PACU. The nurse performs a baseline assessment, then checks
the surgical site for drainage or hemorrhage and makes sure that all drainage
tubes and monitoring lines are connected and functioning.
After
the initial assessment, vital signs are monitored and the patient’s general
physical status is assessed at least every 15 minutes. Patency of the airway
and respiratory function are always evalu-ated first, followed by assessment of
cardiovascular function, the condition of the surgical site, and function of
the central nervous system. The nurse needs to be aware of any pertinent
informa-tion from the patient’s history that may be significant (eg, patient is
hard of hearing, has a history of seizures, has diabetes, or is allergic to
certain medications or to latex).
Maintaining a Patent Airway
The
primary objective in the immediate postoperative period is to maintain
pulmonary ventilation and thus prevent hypoxemia (reduced oxygen in the blood)
and hypercapnia (excess carbon dioxide in the blood). Both can occur if the
airway is obstructed and ventilation is reduced (hypoventilation). Besides
checking the physician’s orders for and administering supplemental oxy-gen, the
nurse assesses respiratory rate and depth, ease of respira-tions, oxygen
saturation, and breath sounds (Litwack, 1999; Meeker & Rothrock, 1999).
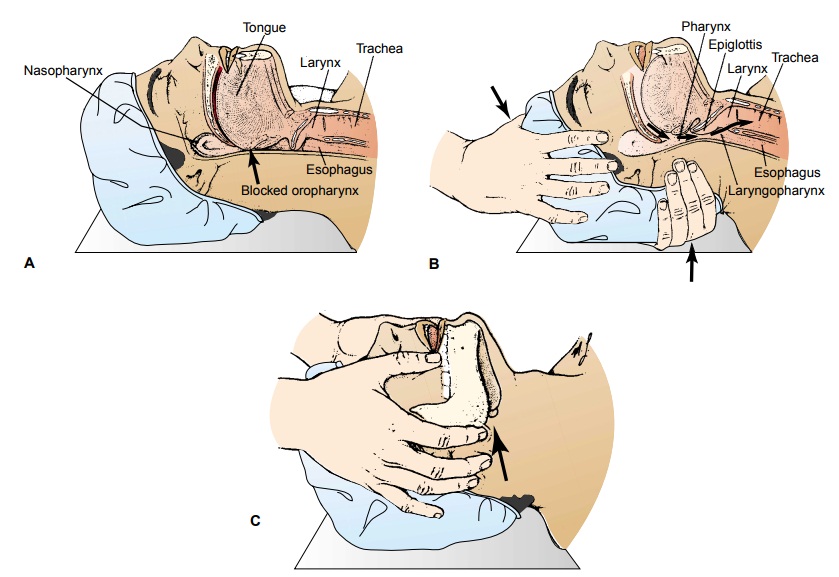
Patients
who have experienced prolonged anesthesia usually are unconscious, with all
muscles relaxed. This relaxation extends to the muscles of the pharynx. When
the patient lies on his or her back, the lower jaw and the tongue fall backward
and the air pas-sages become obstructed (Fig. 20-1A). This is called hypopha-ryngeal obstruction. Signs of occlusion
include choking, noisy and irregular respirations, decreased oxygen saturation
scores, and within minutes a blue, dusky color (cyanosis) of the skin. Because
movement of the thorax and the diaphragm does not necessarily indicate that the
patient is breathing, the nurse needs to place the palm of the hand at the
patient’s nose and mouth to feel the ex-haled breath.
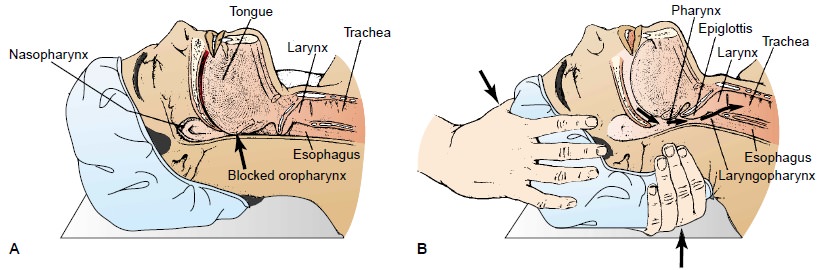
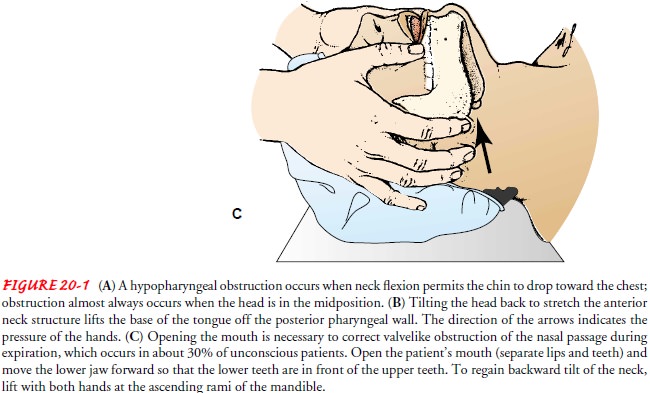
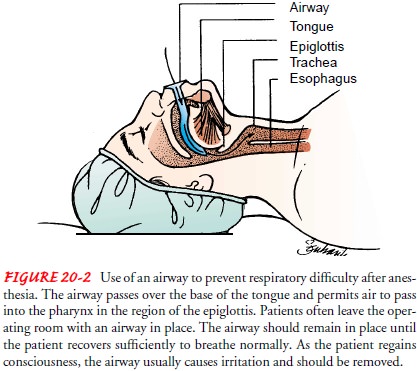
The
anesthesiologist or anesthetist may leave a hard rubber or plastic airway in
the patient’s mouth (Fig. 20-2) to maintain a patent airway. Such a device
should not be removed until signs such as gagging indicate that reflex action
is returning. Alterna-tively, the patient may enter the PACU with an
endotracheal tube still in place and may require continued mechanical
ventilation. The nurse assists in initiating the use of the ventilator and in
the weaning and extubation processes. Some patients, particularly those who
have had extensive or lengthy surgical procedures, may be transferred from the
operating room directly to the intensive care unit or may be transferred from
the PACU to the intensive care unit while still intubated and on mechanical
ventilation.
Respiratory
difficulty can also result from excessive secretion of mucus or aspiration of
vomitus. Turning the patient to one side allows the collected fluid to escape
from the side of the mouth. If the teeth are clenched, the mouth may be opened
man-ually but cautiously with a padded tongue depressor. The head of the bed is
elevated 15 to 30 degrees unless contraindicated, and the patient is closely
observed to maintain the airway as well as to minimize the risk of aspiration.
If vomiting occurs, the patient is turned to the side to prevent aspiration and
the vomitus is col-lected in the emesis basin. Mucus or vomitus obstructing the
pharynx or the trachea is suctioned with a pharyngeal suction tip or a nasal
catheter introduced into the nasopharynx or orophar-ynx. The catheter can be
passed into the nasopharynx or orophar-ynx safely to a distance of 15 to 20 cm
(6 to 8 inches). Caution is necessary in suctioning the throat of a patient who
has had a ton-sillectomy or other oral or laryngeal surgery because of risk for
bleeding and discomfort.
Maintaining Cardiovascular Stability
To
monitor cardiovascular stability, the nurse assesses the pa-tient’s mental
status; vital signs; cardiac rhythm; skin tempera-ture, color, and moisture;
and urine output. Central venous pressure, pulmonary artery pressure, and
arterial lines are moni-tored if the patient’s condition requires such
assessment. The nurse also assesses the patency of all IV lines. The primary
cardio-vascular complications seen in the PACU include hypotension and shock,
hemorrhage, hypertension, and dysrhythmias.
HYPOTENSION AND SHOCK
Hypotension
can result from blood loss, hypoventilation, posi-tion changes, pooling of
blood in the extremities, or side effects of medications and anesthetics; the
most common cause is loss of circulating volume through blood and plasma loss.
If the amount of blood loss exceeds 500 mL (especially if the loss is rapid),
re-placement is usually indicated.
Shock, one of the most serious postoperative complications, can result from hypovolemia. Shock may be described as inadequate cellular oxygenation accompanied by the inability to excrete waste products of metabolism. Hypovolemic shock is characterized by a fall in venous pressure, a rise in peripheral resistance, and tachy-cardia. Neurogenic shock, a less common cause of shock in the sur-gical patient, occurs as a result of decreased arterial resistance caused by spinal anesthesia. It is characterized by a fall in blood pressure due to pooling of blood in dilated capacitance vessels (those with the ability to change volume capacity). Cardiogenic shock is unlikely in the surgical patient except if the patient has se-vere preexisting cardiac disease or experienced a myocardial in-farction during surgery.
The classic signs of shock are:
• Pallor
• Cool, moist skin
• Rapid breathing
• Cyanosis of the lips, gums, and tongue
• Rapid, weak, thready pulse
• Decreasing pulse pressure
• Low blood pressure and concentrated urine
Hypovolemic
shock can be avoided largely by the timely ad-ministration of IV fluids, blood,
blood products, and medica-tions that elevate blood pressure. Other factors may
contribute to hemodynamic instability, and the PACU nurse implements mul-tiple
measures to manage these factors. Pain is controlled by mak-ing the patient as
comfortable as possible and by using opioids judiciously. Exposure is avoided,
and normothermia is main-tained to prevent vasodilation.
Volume
replacement is the primary intervention for shock. An infusion of lactated
Ringer’s solution or blood component ther-apy is initiated. Oxygen is administered
by nasal cannula, face-mask, or mechanical ventilation. Cardiotonic,
vasodilator, and corticosteroid medications may be prescribed to improve
cardiac function and reduce peripheral vascular resistance. The patient is kept
warm while avoiding overheating to prevent cutaneous ves-sels from dilating and
depriving vital organs of blood. The patient is placed flat in bed with the
legs elevated. Respiratory and pulse rate, blood pressure, blood oxygen
concentration, urinary output, level of consciousness, central venous pressure,
pulmonary artery pressure, pulmonary capillary wedge pressure, and cardiac
output are monitored to provide information on the patient’s respiratory and
cardiovascular status. Vital signs are monitored continuously until the patient’s
condition has stabilized.
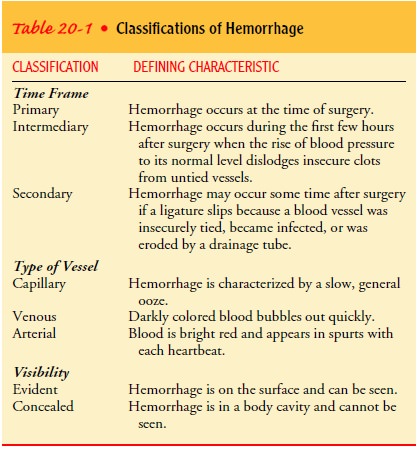
HEMORRHAGE
Hemorrhage
is an uncommon yet serious complication of surgery that can result in death
(Finkelmeier, 2000). It can present in-sidiously or emergently at any time in
the immediate postopera-tive period or up to several days after surgery (Table
20-1). When blood loss is extreme, the patient is apprehensive, restless, and
thirsty; the skin is cold, moist, and pale. The pulse rate increases, the
temperature falls, and respirations are rapid and deep, often of the gasping
type spoken of as “air hunger.” If hemorrhage pro-gresses untreated, cardiac
output decreases, arterial and venous blood pressure and hemoglobin level fall
rapidly, the lips and the conjunctivae become pallid, spots appear before the
eyes, a ring-ing is heard in the ears, and the patient grows weaker but remains
conscious until near death.
Transfusing
blood or blood products and determining the cause of hemorrhage are the initial
therapeutic measures. The sur-gical site and incision should always be inspected
for bleeding. If bleeding is evident, a sterile gauze pad and a pressure
dressing are applied, and the site of the bleeding is elevated to heart level
if possible. The patient is placed in the shock position (flat on back; legs
elevated at a 20-degree angle; knees kept straight). If the source of bleeding
is concealed, the patient may be taken back to the operating room for emergency
exploration of the surgical site.
Special
considerations must be given to patients who decline blood transfusions, such
as Jehovah’s Witnesses and those who identify specific requests on their
advance directives or living will.
HYPERTENSION AND DYSRHYTHMIAS
Hypertension
is common in the immediate postoperative period secondary to sympathetic
nervous system stimulation from pain, hypoxia, or bladder distention.
Dysrhythmias are associated with electrolyte imbalance, altered respiratory
function, pain, hypo-thermia, stress, and anesthetic medications. Both
conditions are managed by treating the underlying causes.
Relieving Pain and Anxiety
Opioid
analgesics are administered judiciously and often intra-venously in the PACU
(Meeker & Rothrock, 1999). Intravenous opioids provide immediate relief and
are short-acting, thus min-imizing the potential for drug interactions or
prolonged respira-tory depression while anesthetics are still active in the
patient’s system. In addition to monitoring the patient’s physiologic sta-tus
and managing pain, the PACU nurse provides psychological support in an effort
to relieve the patient’s fears and concerns. The nurse checks the medical
record for special needs and con-cerns of the patient. When the patient’s
condition permits, a close member of the family may visit in the PACU for a few
moments. This often decreases the family’s anxiety and makes the patient feel
more secure.
Controlling Nausea and Vomiting
Nausea
and vomiting are common problems in the PACU. The nurse should intervene at the
patient’s first report of nausea to con-trol the problem rather than wait for
it to progress to vomiting.
Many
medications are available to control nausea and vomit-ing without oversedating
the patient; they are commonly ad-ministered during surgery as well as in the
PACU (Meeker & Rothrock, 1999). Intravenous or intramuscular administration
of droperidol (Inapsine) is common, especially in the ambulatory setting. Other
medications such as metoclopramide (Reglan), prochlorperazine (Compazine), and
promethazine (Phenergan) are commonly prescribed (Karch, 2002; Meeker &
Rothrock, 1999). Although it is costly, ondansetron (Zofran) is a frequently
used, effective antiemetic with few side effects.
Gerontologic Considerations
The
elderly patient, like all other patients, is transferred from the operating
room table to the bed or stretcher slowly and gently. The effects of this
action on blood pressure and ventilation are monitored. Special attention is
given to keeping the patient warm because the elderly are more susceptible to
hypothermia. The pa-tient’s position is changed frequently to stimulate
respirations and to promote circulation and comfort.
Immediate
postoperative care for the elderly patient is the same as that for any surgical
patient, but additional support is given if there is impaired cardiovascular,
pulmonary, or renal function. With invasive monitoring, it is possible to
detect cardio-pulmonary deficits before signs and symptoms are apparent. The
elderly patient has less physiologic reserve, and physiologic re-sponses to
stress are diminished or slowed. These changes re-inforce the need for close
monitoring and prompt treatment of hypotension, shock, and hemorrhage. Because
of monitoring and improved individualized preoperative preparation, many older
adults tolerate surgery well and have an uneventful recovery.
Postoperative
confusion is common in older patients. The confusion is aggravated by social
isolation, restraints, anesthetics and analgesics, and sensory deprivation.
Reorienting the patient to the environment and using smaller amounts of
sedatives, anes-thetics, and analgesics may help prevent confusion. However,
un-relieved pain, particularly pain at rest, may increase the risk for delirium
and must be addressed (Lynch, Lazor, Gellis et al., 1998). Hypoxia can present
as confusion and restlessness, as can blood loss and electrolyte imbalance.
Excluding all other causes of confusion must precede the assumption that
confusion is re-lated to age, circumstances, and medications.
Determining Readiness for Discharge From the PACU
A patient remains in the PACU until he or she has fully recov-ered from the anesthetic agent (Meeker & Rothrock, 1999). Indicators of recovery include stable blood pressure, adequate res-piratory function, adequate oxygen saturation level compared with baseline, and spontaneous movement or movement on com-mand. Usually the following measures are used to determine the patient’s readiness for discharge from the PACU:
·
Stable vital signs
·
Orientation to person, place,
events, and time
·
Uncompromised pulmonary function
·
Pulse oximetry readings indicating
adequate blood oxygen saturation
·
Urine output at least 30 mL/h
·
Nausea and vomiting absent or under
control
·
Minimal pain
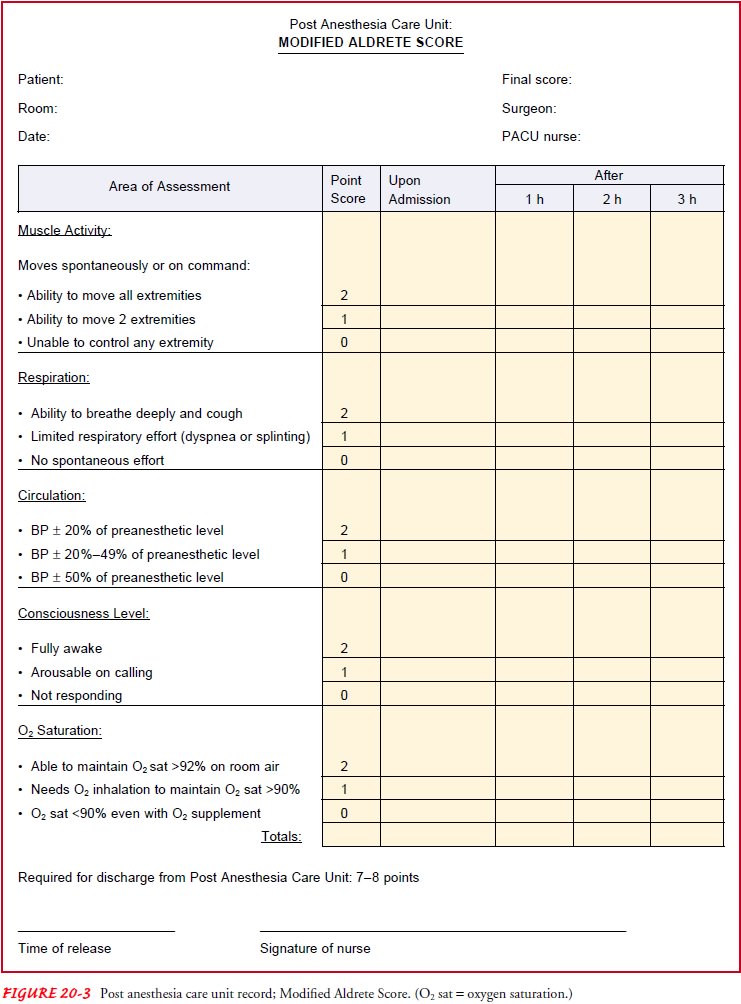
Many hospitals use a scoring system (eg, Aldrete score) to de-termine the patient’s general condition and readiness for transfer from the PACU (Quinn, 1999). Throughout the recovery pe-riod, the patient’s physical signs are observed and evaluated by means of a scoring system based on a set of objective criteria. This evaluation guide, a modification of the Apgar scoring system used for evaluating newborns, allows a more objective assessment of the patient’s condition in the PACU (Fig. 20-3). The patient is assessed at regular intervals (eg, every 15 or 30 minutes), and the score is totaled on the assessment record. Patients with a score lower than 7 must remain in the PACU until their condition improves or they are transferred to an intensive care area, depend-ing on their preoperative baseline scores.
The
patient is discharged from the phase I PACU by the anes-thesiologist or
anesthetist to the critical care unit, the medical-surgical unit, the phase II
PACU, or home with a responsible family member (Quinn, 1999). Patients being
discharged directly to home require verbal and written instructions and
information about follow-up care.
Promoting Home and Community-Based Care
To
ensure patient safety and recovery, expert patient teaching and discharge
planning are necessary when a patient undergoes same-day or ambulatory surgery.
Because anesthetics cloud memory for concurrent events, instructions should be
given to both the pa-tient and the adult who will be accompanying the patient
home (Quinn, 1999).
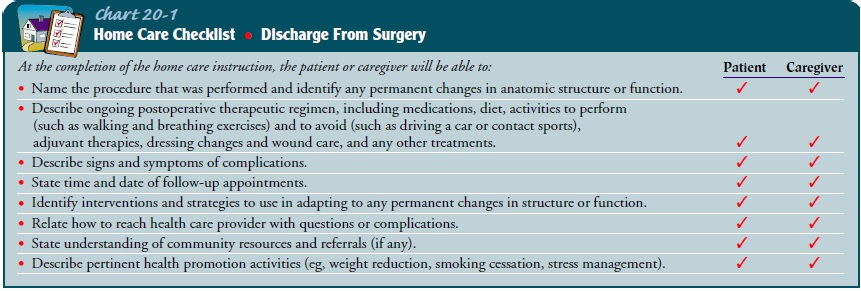
TEACHING PATIENTS SELF-CARE
The
patient and caregiver (eg, family member or friend) are in-formed about
expected outcomes and immediate postoperative changes anticipated in the
patient’s capacity for self-care (Fox, 1998; Quinn, 1999). Written instructions
about wound care, ac-tivity and dietary recommendations, medication, and
follow-up visits to the same-day surgery unit or the surgeon are provided.
Written instructions (designed to be copied and given to patients) about the
postoperative care following many types of surgery are usually provided
(Economou & Economou, 1999). The patient’s caregiver at home is provided
with verbal and written instructions about what to observe the patient for and
about the actions to take if complications occur. Prescriptions are given to
the patient. The nurse or surgeon’s telephone number is provided, and the
patient and caregiver are encouraged to call with questions and to schedule
follow-up appointments (Chart 20-1).
Although
recovery time varies depending on the type and ex-tent of surgery and the
patient’s overall condition, instructions usually advise limited activity for
24 to 48 hours. During this time, the patient should not drive a vehicle, drink
alcoholic bev-erages, or perform tasks that require energy or skill. Fluids may
be consumed as desired, and smaller-than-normal amounts are eaten at mealtime.
The patient is cautioned not to make impor-tant decisions at this time because
the medications, anesthesia, and surgery may affect his or her decision-making
ability.
CONTINUING CARE
Although most patients who undergo ambulatory surgery re-cover quickly and without complications, some patients require referral for home care. These may be elderly or frail patients, those who live alone, and patients with other health care prob-lems that may interfere with self-care or resumption of usual ac-tivities. The home care nurse assesses the patient’s physical status (eg, respiratory and cardiovascular status, adequacy of pain management, the surgical incision) and the patient’s and family’s ability to adhere to the recommendations given at the time of discharge. Previous teaching is reinforced as needed. The home care nurse may change surgical dressings, monitor the pa-tency of a drainage system, or administer medications. The pa-tient is assessed for any surgical complications. The patient and family are reminded about the importance of keeping follow-up appointments with the surgeon. Follow-up phone calls from the nurse or surgeon may also be used to assess the patient’s progress and to answer any questions (Fox, 1998; Marley & Swanson, 2001).
Related Topics