Chapter: Medical Surgical Nursing: Postoperative Nursing Management
The Hospitalized Postoperative Patient
The Hospitalized Postoperative Patient
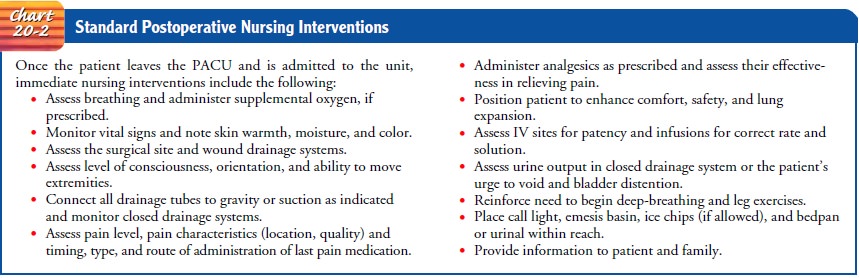
The patient admitted to the clinical unit for postoperative care has multiple needs. Seriously ill patients or those who have un-dergone major cardiovascular, pulmonary, or neurologic surgery are admitted to specialized intensive care units for close moni-toring and advanced interventions and support. The care re-quired by these patients in the immediate postoperative period. Postoperative care for the surgical patient returning to the general medical-surgical unit is discussed below.
RECEIVING THE PATIENT IN THE CLINICAL UNIT
The
patient’s room is readied by assembling the necessary equip-ment and supplies:
IV pole, drainage receptacle holder, emesis basin, tissues, disposable pads
(Chux), blankets, and postopera-tive charting forms. When the call comes to the
unit about the patient’s transfer from the PACU, the need for any additional
items that may be needed is communicated. The PACU nurse re-ports the baseline
data about the patient’s condition to the re-ceiving nurse. The report includes
demographic data, medical diagnosis, procedure performed, comorbid conditions,
allergies, unexpected intraoperative events, estimated blood loss, the type and
amount of fluids received, medications administered for pain, whether the
patient has voided, and information that the patient and family have received
about the patient’s condition. Usually the surgeon speaks to the family after
surgery and relates the general condition of the patient. The receiving nurse
reviews the postoperative orders, admits the patient to the unit, performs an
initial assessment, and attends to the patient’s immediate needs (Chart 20-2).
NURSING MANAGEMENT AFTER SURGERY
During the first 24 hours after surgery,
nursing care of the hos-pitalized patient on the general medical-surgical unit
involves continuing to help the patient recover from the effects of anesthesia,
frequently assessing the patient’s physiologic status, mon-itoring for
complications, managing pain, and implementing measures designed to achieve the
long-range goals of indepen-dence with self-care, successful management of the
therapeutic regimen, discharge to home, and full recovery. In the initial hours
after admission to the clinical unit, adequate ventilation, hemo-dynamic
stability, incisional pain, surgical site integrity, nausea and vomiting,
neurologic status, and spontaneous voiding are primary concerns. The pulse
rate, blood pressure, and respiration rate are recorded at least every 15
minutes for the first hour and every 30 minutes for the next 2 hours.
Thereafter, they are mea-sured less frequently if they remain stable. The
temperature is monitored every 4 hours for the first 24 hours.
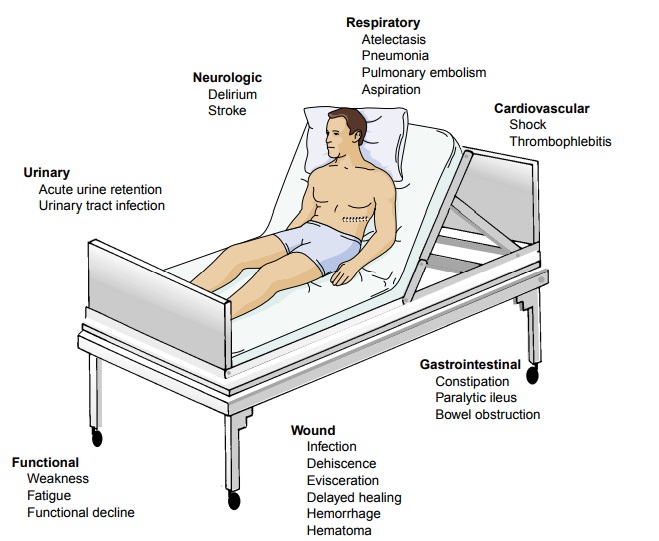
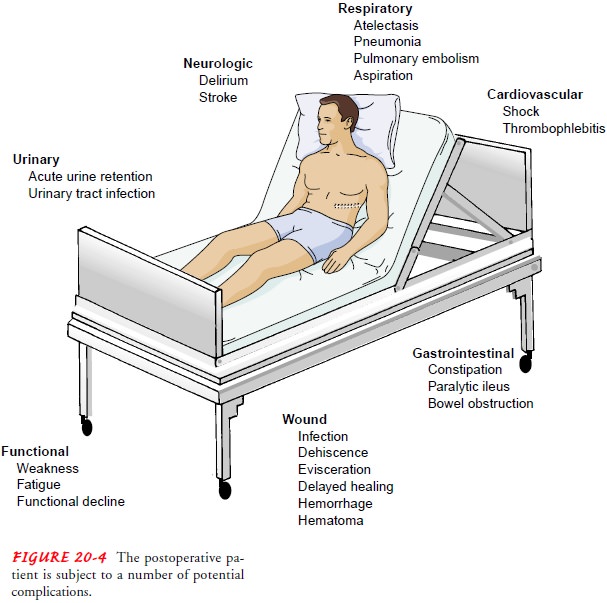
Patients
usually begin to feel better several hours after surgery or after waking up the
next morning. Although pain may still be intense, many patients feel more
alert, less nauseous, and less anx-ious. They have begun their breathing and
leg exercises, and many will have dangled their legs over the edge of the bed,
stood, and ambulated a few feet or been assisted out of bed to the chair at
least once. Many will have tolerated a light meal and had IV fluids
discontinued. The focus of care shifts from intense physi-ologic management and
symptomatic relief of the adverse ef-fects of anesthesia to regaining
independence with self-care and preparing for discharge. Despite these gains,
the postoperative pa-tient is still at risk for complications. Atelectasis,
pneumonia, deep vein thrombosis, pulmonary embolism, constipation, para-lytic
ileus, and wound infection are ongoing threats for the post-operative patient
(Fig. 20-4).
Related Topics