Chapter: Essentials of Psychiatry: Medication-induced Movement Disorders
Neuroleptic Malignant Syndrome
Neuroleptic
Malignant Syndrome
Etiology and Pathophysiology
Neuroleptic
Malignant Syndrome (NMS) is a potentially fatal reaction to antipsychotic
medications that is characterized clini-cally by muscle rigidity, fever,
autonomic instability and changes in level of consciousness. The
pathophysiological mechanism of NMS remains unclear. The hypothesis of most
interest is that of reduced dopaminergic activity secondary to
neuroleptic-induced dopamine blockade. This reduced dopamine activity in
differ-ent parts of the brain (hypothalamus, nigrostriatal system and
corticolimbic tracts) may serve to explain the various clinical features of
NMS. Dopamine reduction in the hypothalamus may cause fever and autonomic
instability; in the nigrostriatal system, dopamine reduction may lead to the
rigidity; and the reduction in corticolimbic dopamine activity may explain the
altered con-sciousness. This hypothesis is based on the fact that
antipsychot-ics are dopamine-blocking agents, whereas certain dopamine agonists
are reported to help resolve NMS.
The
dopaminergic blocking theory does not, however, ex-plain why NMS may develop at
a given time and in a given pa-tient. There are probably other genetic
(possibly a predisposition similar to that seen in malignant hyperthermia),
constitutional, environmental, and pharmacological factors that interact to
pro-duce the syndrome. A number of investigators have proposed that other
neurotransmitter abnormalities may be responsible for the syndrome, including
serotonergic hyperfunction in the hypotha-lamus, excessive catecholamine
secretion, and gamma-aminobu-tyric acid deficiency.
Epidemiology and Comorbidity
The exact
frequency of NMS is unknown. A number of retrospec-tive and prospective studies
have found 0.02 to 3.2% of patients treated with antipsychotics to be affected
with NMS. Several factors probably account for this large variability in
frequency, including differences in study methods and diagnostic criteria for
NMS. A prior episode of NMS appears to predispose to future episodes of NMS.
Any preexisting medical problems, especially those associated with agitation or
dehydration, may increase the likelihood of NMS development when antipsychotics
are used. Patients with a neurological condition as well as patients with
presumed psychosis due to human immunodeficiency virus in-fection may be at
higher risk for development of NMS. A number of potential risk factors related
to antipsychotic treatment have been identified. Higher doses of antipsychotic,
rapid increases in dosage (especially “rapid neuroleptization”) and
intramuscular injections of high-potency conventional agents (e.g., haloperidol
and fluphenazine) have been reported to be risk factors for NMS. NMS can occur
(but rarely) in patients prescribed atypical an-tipsychotics and a review of
atypical-induced NMS concluded that symptoms appear similar to NMS induced by
conventional antipsychotics.
NMS is
more frequently reported in men than in women and is more frequently seen in a
younger population. A previous diagnosis of a mood disorder may place patients
at a higher risk for NMS. Warm, humid climates may also predispose to the
dis-order (American Psychiatric Association, 2000).
Assessment and Differential Diagnosis
NMS
usually presents in the first month of antipsychotic treat-ment but may develop
at any time. Two-thirds of the cases mani-fest within the first week of
treatment (American Psychiatri
Association,
2000). The two key diagnostic features for the dis-order are severe muscle
rigidity (classically referred to as lead pipe rigidity) and elevated
temperature. A number of other fea-tures are also seen (see DSM-IV-TR
criteria). For the psychiatrist, the most suggestive features are fluctuating
consciousness (from confusion to coma), labile vital signs (tachycardia,
unstable or elevated blood pressure), laboratory evidence of muscle injury
(elevation of creatine kinase) and leukocytosis. Other features include
diaphoresis, dysphagia, tremor, incontinence and mutism (American Psychiatric
Association, 2000).
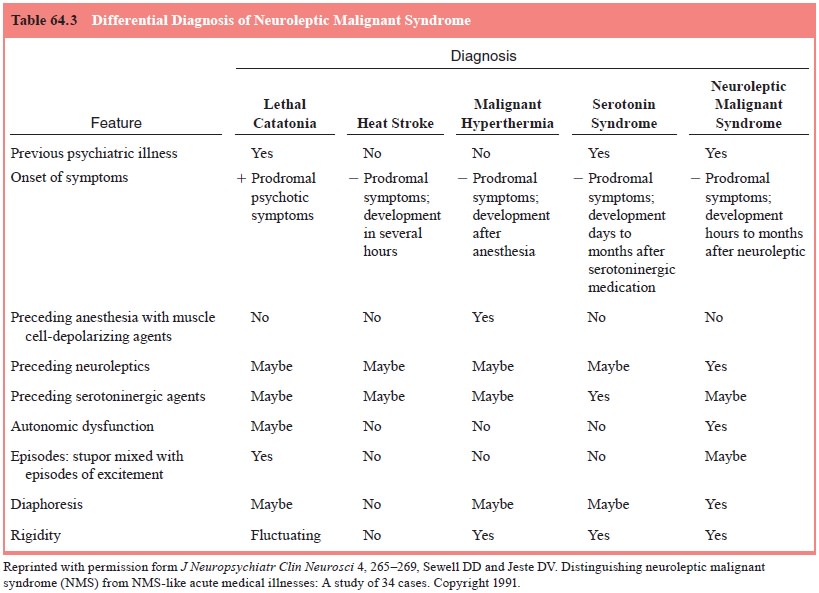
The
differential diagnosis of NMS can be difficult (Table 64.3). The most important
point is that the psychiatrist must start by suspecting NMS and then carefully
rule out other possible organic problems. Because medical illness is a likely
predisposing factor, it is important to consider that NMS may be present even
if a definitive organic disease is found to explain the NMS-like symptoms.
Numerous
general medical and neurological conditions can present with symptoms that may
resemble NMS. Examples include central nervous system infection, status
epilepticus, subcortical brain lesions, porphyria and tetanus (American
Psychiatric Associ-ation, 2000). The presence of significantly elevated
temperature and severe muscle rigidity makes the diagnosis of NMS more likely.
The
syndrome of lethal catatonia (seen in patients with uncontrolled manic
excitement or catatonic schizophrenia) can mimic NMS (with increased
temperature, autonomic irregu-larities and elevated creatine kinase), and the
differential di-agnosis can be difficult. It is obviously important to
determine whether the patient is indeed being treated with an antipsychotic. Although
NMS may clinically look like catatonia, NMS does not typically have alternating
periods of catatonic excitement and catatonic mutism. A past history of
catatonic episodes is also im-portant in making the differential diagnosis.
Lorazepam may be useful in alleviating the symptoms of catatonia but it has not
been shown to be useful in treatment of NMS. Therefore, it is possible that a
brief lorazepam trial could provide a useful and relatively easy method of
distinguishing between these two conditions. The problem, of course, is that
not all cases of catatonia respond to lorazepam.
Heat
stroke may also look like NMS but typically differs in that it presents with
hypotension, dry skin and limb flaccid-ity (American Psychiatric Association,
2000). Malignant hyper-thermia can also have a similar presentation but
generally occurs within the context of a patient’s receiving halogenated
anesthetic agents or succinylcholine. This condition typically begins
im-mediately after administration of the anesthetic agent and only in
genetically susceptible individuals (American Psychiatric Association, 2000).
Medications
can cause a number of conditions that may present as syndromes similar to NMS.
Allergic drug reactionsmay produce fever and autonomic instability but not
rigidity. Se-rotonin syndrome, with common clinical characteristics includ-ing
fever, resting tremor, rigidity, myoclonus and generalized seizures should also
be considered. A medication history can usually help distinguish between the
two syndromes, but patients receiving antipsychotics may also be treated with
selective sero-tonin reuptake inhibitors, thus making the clinical picture more
confusing. Lithium intoxication and anticholinergic delirium can both resemble
NMS, as can intoxication with amphetamines, co-caine and phencyclidine as well
as rapid termination of antipar-kinsonian medication.
Course
The
course of NMS is variable. Some cases may progress to fatal-ity, whereas others
may follow a mild self-limited course. Once the syndrome is recognized and the
antipsychotic medication is discontinued, the syndrome usually resolves between
2 weeks and 1 month (American Psychiatric Association, 2000).
Mortality
rate is reported to be 4 to 25%. The most com-mon medical complications leading
to morbidity and mortality are respiratory failure and renal failure. Shalev
and coworkers (1989) reported that myoglobinemia and renal failure are the best
predictors of mortality in NMS; the presence of either condition imparted a 50%
mortality risk. In general, complications are a result of physiologic
consequences of severe rigidity and immo-bilization such as deep vein
thrombosis, pulmonary embolism, dehydration and an increased risk for
rhabdomyolysis.
Treatment
The most
critical step in treatment (Table 64.4) is to recognize the clinical features
of the syndrome and rapidly discontinue the an-tipsychotic. The importance of
this initial step mandates that psy-chiatrists who use antipsychotics in their
practice be cognizant of the early clinical features and recognize that the
syndrome can occur at any time during the course of treatment. Once the
an-tipsychotic has been stopped, supportive care remains the core of treatment
and often must be carried out in the context of a medical intensive care unit.
Each supportive intervention should be targeted to a specific symptom. Examples
of interventions in-clude cooling blankets for fever, cardiac monitoring for
arrhyth-mias, parenteral hydration for dehydration and monitoring for urine
output and renal function. Dialysis may also be considered for acute renal
failure.
It should
be noted that despite their widespread use, the efficacy of the muscle relaxant
dantrolene and the dopamine agonist bromocriptine has not been thoroughly
established. Electroconvulsive therapy is another treatment option in NMS
presumably because it increases dopamine turnover in the brain.
Electroconvulsive therapy is particularly indicated when there is difficulty in
distinguishing between NMS and lethal catatonia and when there seems to be a
significant risk of recurrence of NMS on restarting neuroleptics. Some
psychiatrists report rapid
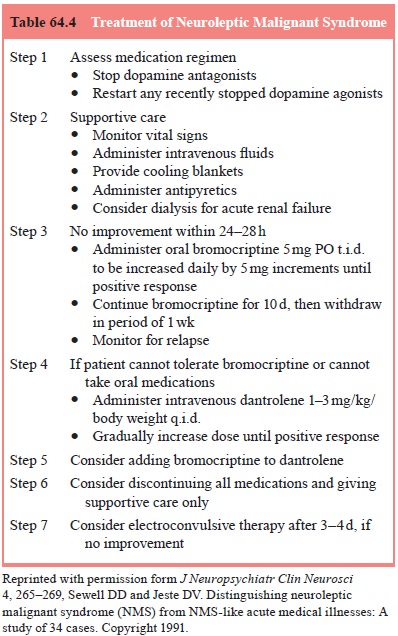
and
dramatic success in the use of electroconvulsive therapy for NMS.
At
present, the appropriate course is to begin with antipsy-chotic discontinuation
and supportive care and to consider anti-dote therapy only if improvement in
symptoms is not seen within the first few days. The treatment of NMS should be
individual-ized for each patient based on clinical signs and symptoms. For example,
supportive care may be sufficient in mild and early cases of NMS. Trials of
bromocriptine, dantrolene, or amantadine are suggested for patients with
moderate symptoms. Anticholiner-gics can be used in managing afebrile patients
with neuroleptic-induced parkinsonian symptoms and benzodiazepines may be
useful for agitation in NMS. ECT is recommended in situations where lethal
catatonia is suspected, when NMS symptoms are treatment refractory, and in
patients who remain psychotic in the immediate post-NMS period.
A
particular difficulty for the psychotic patient who has NMS is that rechallenge
with antipsychotics may cause NMS to recur. Successful rechallenge seems to be
positively related to the length of time elapsed after resolution of NMS. There
is some evidence to suggest that clozapine may have relatively little
propensity to induce NMS. Clozapine, therefore, may represent one option for
the patient who has experienced NMS with a con-ventional agent. It is likely
but not yet known definitively that atypical antipsychotics will prove to have
a lower frequency of NMS. In general, it is recommended to switch to an agent
in a different chemical class and with a lower D2 affinity compared
with the causal agent.
Related Topics