Chapter: Obstetrics and Gynecology: Maternal-Fetal Physiology
Maternal Physiology: Cardiovascular System
MATERNAL PHYSIOLOGY
Cardiovascular System
The
earliest and most dramatic changes in maternal physiology are cardiovascular. These
changes improve fetal oxygena-tion and nutrition.
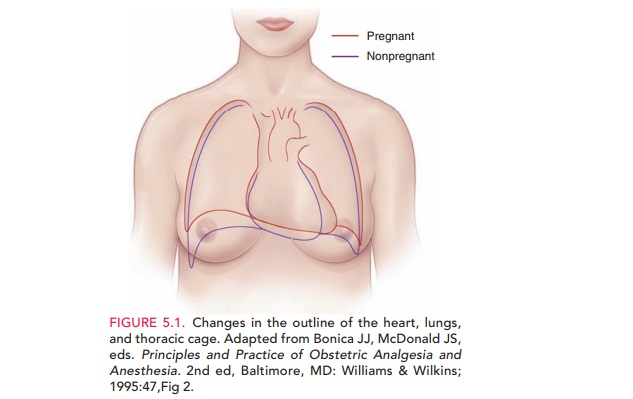
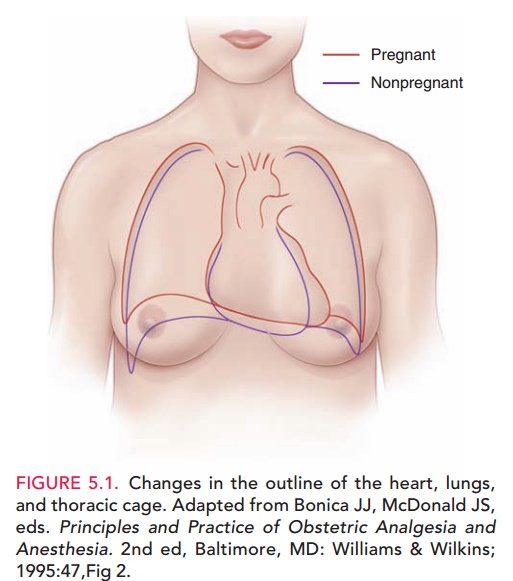
ANATOMIC CHANGES
During pregnancy, the heart is
displaced upward and to the left and assumes a more horizontal position as its
apex is moved laterally (Fig. 5.1). These position changes are the result of
diaphragmatic elevation caused by displace-ment of abdominal viscera by the
enlarging uterus. In addition, ventricular muscle mass increases and both the
left ventricle and atrium increase in size parallel with an increase in
circulating blood volume.
FUNCTIONAL CHANGES
The
primary functional change in the cardiovascular system in pregnancy is a marked
increase in cardiac output.
Overall, cardiac output increases
30% to 50%, with 50% of that increase occurring by 8 weeks’ gestation. In the
first half of pregnancy, cardiac output rises as a result of increased stroke
volume, and in the latter half of preg-nancy, as a result of increased maternal
heart rate while the stroke volume returns to near-normal, nonpregnant levels.
These changes in stroke volume are due to alter-ations in circulating blood
volume and systemic vascular resistance. Circulating blood volume begins
increasing by 6 to 8 weeks’ gestation and reaches a peak increase of 45% by 32
weeks’ gestation. Systemic vascular resistance decreases because of a
combination of the smooth muscle-relaxing effect of progesterone, increased
production of vasodilatory substances (prostaglandins, nitric oxide, atrial
natriuretic peptide), and arteriovenous shunting to the uteroplacental
circulation.
However, late in pregnancy,
cardiac output may decrease when venous return to the heart is impeded because
of vena caval obstruction by the enlarging gravid uterus. At times, in term
pregnancy, nearly complete occlu-sion of the inferior vena cava occurs,
especially in the supine position, with venous return from the lower
extremities shunted primarily through the dilated paravertebral collat-eral
circulation.
The distribution of the enhanced
cardiac output varies during pregnancy. The uterus receives about 2% of the
cardiac output in the first trimester, increasing to up to 20% at term, mainly
by means of a relative reduction of the fraction of cardiac output that goes to
the splanchnic bed and skeletal muscle. However, the absolute blood flow to
these areas does not change, because of the increase in cardiac output that
occurs in late pregnancy.
During pregnancy, arterial blood
pressure follows a typical pattern. When measured in the sitting or stand-ing
position, diastolic blood pressure decreases begin-ning in the 7th week of
gestation and reaches a maximal decline of 10 mm Hg from 24 to 32 weeks. Blood
pres-sure then gradually returns to nonpregnant values by term. Resting
maternal pulse increases as pregnancy pro-gresses, increasing by 10–18 beats
per minute over the nonpregnant value by term.
During labor, at the time of
uterine contraction, car-diac output increases approximately 40% above that in
late pregnancy, and mean arterial pressure increases by approx-imately 10 mm
Hg. A decline in these parameters follow-ing administration of an epidural
anesthetic suggests that many of these changes are the result of pain and
apprehen-sion. Cardiac output increases significantly immediately after
delivery, because venous return to the heart is no longer blocked by the gravid
uterus impinging on the vena cava and because extracellular fluid is quickly
mobilized.
SYMPTOMS
Although most women do not become
overtly hypoten-sive when lying supine, perhaps one in 10 have symptoms that
include dizziness, light-headedness,
and syncope. These symptoms, often
termed the inferior vena cava syn-drome, may be related to ineffective shunting
via the paravertebral circulation when the gravid uterus occludes the inferior
vena cava.
PHYSICAL FINDINGS
The cardiovascular system is in a
hyperdynamic state dur-ing pregnancy. Normal
physical findings on cardiovascularexamination include an increased second heart sound splitwith inspiration, distended neck
veins, and low-grade sys-tolic
ejection murmurs, which are presumably associated withincreased blood flow
across the aortic and pulmonic valves. Manynormal pregnant women have an S3
gallop, or third heart sound, after midpregnancy. Diastolic murmurs should not
be considered normal in pregnancy.
DIAGNOSTIC TESTS
Serial
blood pressure assessment is an essential component of each prenatal care
visit.
Blood pressure recordings during
pregnancy are influ-enced by maternal position; therefore, a consistent
position should be used during prenatal care, facilitating the recog-nition of
trends in blood pressure during pregnancy and their documentation. Measured blood pressure is highest whena
pregnant woman is seated, somewhat lower when supine, and lowest while lying on
the side. In the lateral recumbent posi-tion, the measured pressure in the
superior arm is about 10 mm Hg lower than that simultaneously measured in the
inferior arm. Blood pressures higher than the nonpregnant values for a
particular patient should be presumed abnor-mal pending evaluation.
The normal anatomic changes of
the maternal heart in pregnancy can produce subtle, but insignificant, changes
in chest radiographs and electrocardiograms. In chest radio-graphs, the cardiac
silhouette can appear enlarged, causing a misinterpretation of cardiomegaly. In
electrocardiograms, a slight left axis deviation may be apparent.
Related Topics