Chapter: Obstetrics and Gynecology: Neoplasia Gestational Trophoblastic
Malignant Gestational Trophoblastic Neoplasia
MALIGNANT GESTATIONAL TROPHOBLASTIC NEOPLASIA
Postmolar or persistent GTD is only one of the many forms of malignant GTD.
Although invasive moles are his-tologically identical to antecedent molar
pregnancies while invading the myometrium, choriocarcinomas
are a malig-nant transformation of trophoblastic tissue. Instead of hydropic
chorionic villi, the tumor has a red granular appearance on cut suction and
consists of intermingled syncytiotrophoblastic and cytotrophoblastic elements
with many abnormal cellular forms. Clinically, choriocarcino-mas are
characterized by rapid myometrial and uterine-vessel invasion and systemic
metastases resulting from hematogenous embolization. Lung, vagina, central
ner-vous system, kidney, and liver are common metastatic loca-tions.
Choriocarcinoma may follow a molar pregnancy, normal-term pregnancy, abortion,
or ectopic pregnancy. In the United States, choriocarcinoma is associated with
approximately 1 in 150,000 pregnancies, 1 in 15,000 abor-tions, 1 in 5000
ectopic pregnancies, and 1 in 40 molar pregnancies.
Early identification and
treatment are important. Abnormal bleeding
for more than 6 weeks after any pregnancy should be evaluated with hCG testing
to exclude a new pregnancy or GTD. Failure of quantitative hCG levels to
regress aftertreatment of a molar pregnancy suggests that further treat-ment is
needed. Identified metastatic sites should not be biopsied to avoid bleeding
complications. Most GTN,including
malignant forms, are highly sensitive to chemotherapy and often results in a
cure, allowing for future reproduction.
Nonmetastatic
persistent GTN is completely treated by single-agent chemotherapy. Single-agent
chemotherapy iseither methotrexate
or actinomycin D. The prognosis for
metastatic GTN is more complex, divided into good and poor prognostic
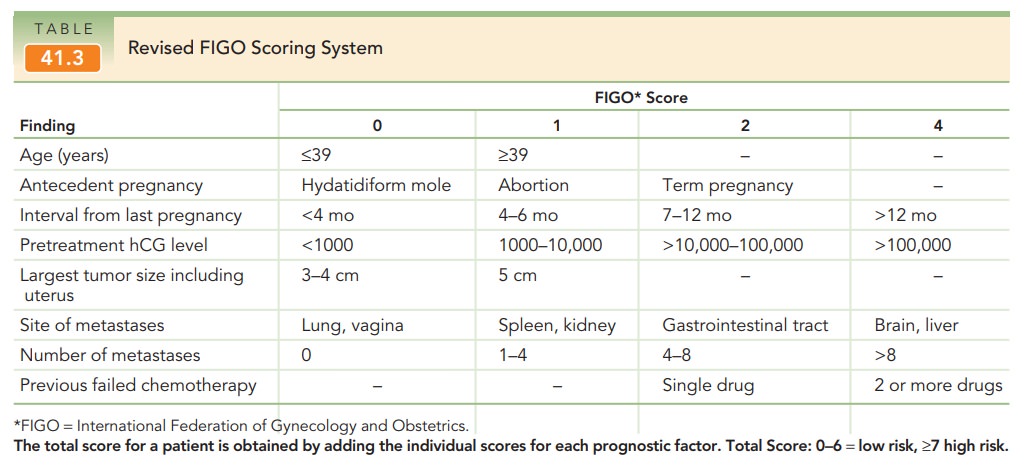
categories (Table 41-2). The World Health Organization (WHO) has developed a
prognostic scoring system for GTN that includes a number of epi-demiologic and
laboratory findings; this system was later combined into the International
Federation of Gynecology and Obstetrics (FIGO) staging system (Table 41-3). A FIGOscore of 7 or above classifies
metastatic GTN as high-risk, requir-ing multi-agent chemotherapy. The
combination chemother-apeutic regimen with the highest success rates is: etoposide,methotrexate, actinomycin D, cyclophosphamide,
andOncovin (vincristine)) [EMACO].
Adjunctive radiother-apy is sometimes performed with patients who have brain or
liver metastasis. Surgery may be necessary to control hem-orrhage, remove
chemotherapy-resistant disease, and treat other complications to stabilize
high-risk patients during intensive chemotherapy. Cure rates for non-metastatic
and good-prognosis metastatic disease approach 100%. Cute rates for
poor-prognosis metastatic disease are 80% to 90%.

Related Topics