Chapter: Obstetrics and Gynecology: Neoplasia Gestational Trophoblastic
Hydatidiform Mole
HYDATIDIFORM MOLE
A hydatidiform mole includes
abnormal proliferation of the syncytiotrophoblast and replacement of normal
pla-cental trophoblastic tissue by hydropic
placental villi.Complete moles do not have identifiable embryonic orfetal
structures. Partial moles are
characterized by focal trophoblastic proliferation, degeneration of the
placenta, and identifiable fetal or embryonic structures.
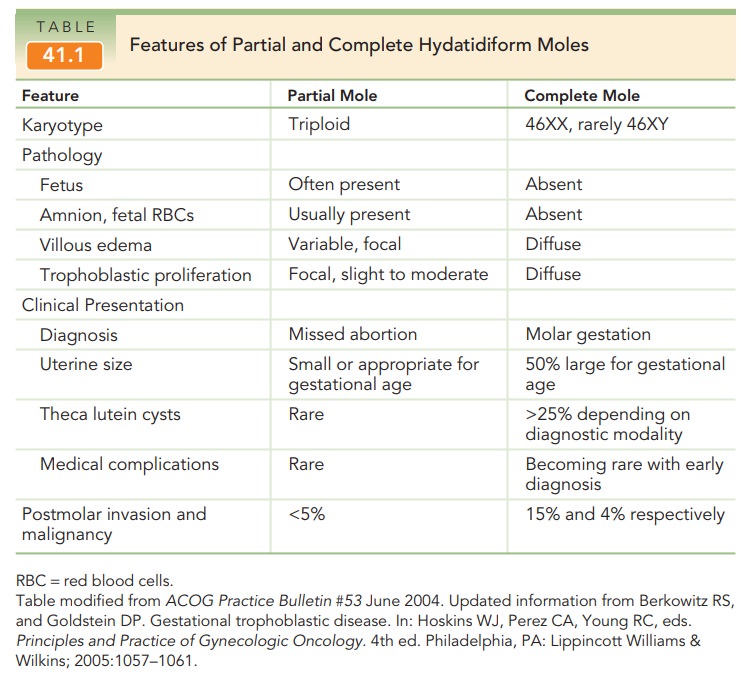
The
genetic constitutions of the two types of molar pregnancy are different (Table
41.1). Complete moles have chromo-somes entirely of paternal origin as the
result of the fer-tilization of a blighted ovum by a haploid sperm that
reduplicates, or rarely, fertilization of a blighted ovum with two sperm. The karyotype of a complete mole is usually
46XX.The fetus of a partial mole is usually a triploid. This consists ofone
haploid set of maternal chromosomes and two haploid sets of paternal
chromosomes, the consequence of di-spermic fertilization of a normal ovum. Complete moles aremore common than partial
moles and are more likely to undergo malignant transformation.
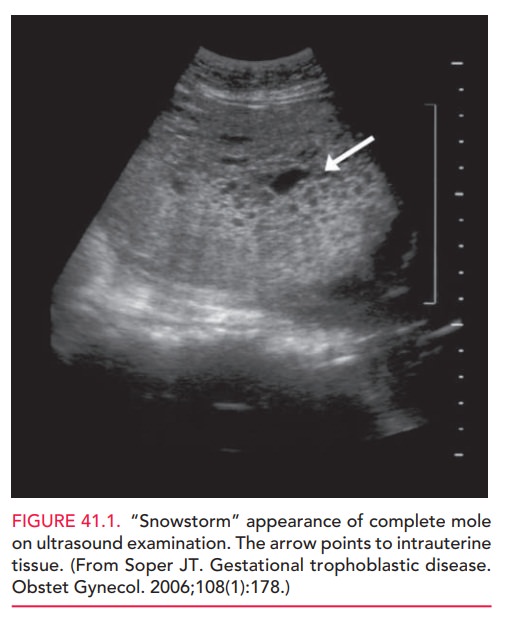
Patients with molar pregnancy have findings consistent with a confirmed pregnancy as well as uterine size and date discrepancy, exaggerated subjective symptoms of preg-nancy, and painless second-trimester bleeding. With theincreased early prevalence of first-trimester ultrasound, moles are now frequently diagnosed in the first trimester of pregnancy before symptoms are present. Abnormal bleeding is the mostcharacteristic presenting symptom which prompts evalu-ation for threatened abortion. Lack of fetal heart tones detected at the first obstetric appointment can also prompt evaluation (depending on the estimated gestational age). Ultrasound imaging confirms the diagnosis of molar preg-nancy by its characteristic “snowstorm” appearance and absence of fetal parts (complete mole) [Fig. 41.1]. In cases of partial mole, ultrasonography reveals an abnormally formed fetus. Quantitative hCG levels are excessively elevated for gestational age, and the uterus is usually larger than expected.
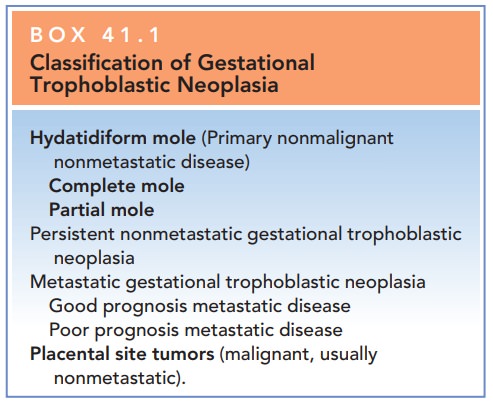
Box 41.1
Classification of Gestational
Trophoblastic
Neoplasia
Hydatidiform
mole (Primary non-malignant nonmetastatic disease)
Complete
mole
Partial
mole
Persistent
nonmetastatic gestational trophoblastic neoplasia
Metastatic
gestational trophoblastic neoplasia
Good
prognosis metastatic disease
Poor prognosis metastatic disease Placental site tumors (malignant, usually nonmetastatic).
Molar pregnancies may present with other signs and symptoms, including severe nausea and vomiting, marked gestational hypertension,
proteinuria, and, rarely, clinical hyperthyroidism. Most of these findings can be attributed tothe high levels of hCG
produced by the abnormal pregnancy. Some patients experience tachycardia
and shortness of breath, arising from intense hemodynamic changes asso-ciated
with acute hypertensive crisis. In these patients physical examination reveals
not only date and size dis-crepancy of the uterine fundus and absent fetal
heart tones, but also changes associated with developing severe hypertension,
such as hyperreflexia. Bimanual pelvic exam-ination may reveal large adnexal
masses (theca luteincysts), which
represent marked enlargement of the ovariessecondary to hCG stimulation.
With earlier diagnosis, the
medical complications of molar pregnancy are becoming less common.
In any
woman who presents with findings suggestive of severe hypertension prior to 20
weeks in pregnancy, a molar pregnancy should be immediately suspected.
Twin pregnancies with a normal
fetus coexisting with a complete or partial mole are exceedingly rare. Women
with these pregnancies should be treated in a tertiary hos-pital center with
specialized care. Medical complications in molar twin gestations rarely allow
these pregnancies to reach term. These pregnancies also have a higher risk of
persistent metastatic or nonmetastatic gestational tro-phoblastic disease
(GTD).
An invasive mole is histologically identical to a com-plete mole. It
invades the myometrium without any inter-vening endometrial stroma seen on
histological sample. It is often diagnosed months after evacuation of a
complete
Whereas
both partial and complete molar pregnancies pre-sent as abnormal pregnancies,
partial mole most often presents as a missed abortion. Vaginal
bleeding is less common in par-tial molar pregnancy than in complete molar
pregnancy. Uterine growth is less than expected for the gestational age in
partial molar pregnancy. Ultrasound reveals molar degeneration of the placenta
and a grossly abnormal fetus or embryo. Medical complications, theca lutein
cysts, and subsequent malignancies are rare (see Table 41-1).
Other
appropriate tests if clinical evidence of hyperthyroidism and/or gestational
hypertension
Treatment
In most
cases of molar pregnancy the definitive treatment is prompt evacuation of the
uterine contents. Uterine evacuationis done most
often by dilation of the cervix, and suction curettage followed by gentle sharp
curettage. Because the evacuation of larger moles is sometimes associated with
uterine atony and excessive blood loss, appropriate prepa-rations should be
made for uterotonic administration and blood transfusion, if needed. In rare
cases of a late present-ing partial molar pregnancy, there may be an additional
need for larger grasping instruments to remove the abnor-mal fetus.
In
general, the larger the uterus, the greater the risk of pul-monary
complications associated with trophoblastic emboli, fluid overload, and anemia.
This is particularly true in
patients with severe associ-ated gestational hypertension, who may experience
con-comitant hemoconcentration and alteration in vascular hemodynamics.
Hysterectomy or induc-tion of labor with prostaglandins is not usually
recom-mended, because of the increased risk of blood loss and other sequelae.
The bilaterally enlarged multicystic ovaries (theca lutein cysts) resulting from follicular stimulation by high
levels of circulating hCG, do not represent malignant changes. The theca lutein cysts invariably regress
within afew months of evacuation, and therefore do not require surgi-cal
removal.
Patients who have no interest in further childbearing or have other indications for hysterectomy may be treated by hysterectomy with ovarian preservation. Despite removal of the entire primary neoplasm, the risk of persistent GTD is 3% to 5%.
Postevacuation Management
Because
of the predisposition for recurrence, patients should be monitored closely for
6 to 12 months after the evacuation of a molar pregnancy. Rh-negative
patients should be given Rh-immune globulin. Follow-up consists of periodic
physical examination to check for vaginal metastasis and appropri-ate
involution of pelvic structures. Quantitative hCG levels should be checked within 48 hours following evacuation,
every 1 to 2 weeks while elevated, and at 1 to 2 months thereafter.
Quantitative hCG levels that rise or reach a plateau are an indication of
persistent disease and the need for further treatment after a new pregnancy has
been ruled out. During the first year,
the patient should be treated withoral contraceptive pills (OCPs) or other
reliable contraceptive method to prevent an intercurrent pregnancy. (Multiple
stud-ies have proven the safety of OCP use after a molar preg-nancy.) The risk
of recurrence after 1 year of remission is<1%. The risk of recurrence with
subsequent pregnancies is 1% to 2%. There is no increase in congenital
anomalies or complications in future pregnancies.
Preoperative Evaluation ofMolar Pregnancy
Baseline quantitative hCG level
Baseline chest x-ray to check for metastatic disease
Complete blood count
Blood type with type and screen
Clotting function studies
Related Topics