Chapter: Obstetrics and Gynecology: Isoimmunization
Isoimmunization: Prevention
PREVENTION
Maternal exposure and subsequent
sensitization to fetal blood usually occurs at delivery, but it can occur at any
time during pregnancy. In the late 1960s, it was discovered that an antibody to
the D antigen of the Rh system could be prepared from donors previously
sensitized to the antigen. Administration of the anti-D immune globulin soon after delivery prevents an active
antibody response to the D anti-gen by the mother in most cases.
Anti-D
immune globulin is effective only for the D antigen of the Rh system. It is not
effective in preventing sensitiza-tion to other Rh antigens or any other red
cell antigens.
It is now standard for Rh
D-negative women who deliver Rh D-positive infants to receive a dose of 300 μg of anti-D immune globulin
within 72 hours of delivery (Box 19.2). This practice reduces the risk of
sensitization to the D antigen from around 16% to approximately 2%. The
residual 2% risk is believed to result from sensitization occurring during the
course of pregnancy, especially dur-ing the third trimester. For this reason, it is standard practiceto
administer a 300-μg dose of anti-D immune globulin
to all Rh D-negative women at about 28 weeks of gestation, unless it is
cer-tain that the father is Rh D-negative. This
prophylactic dosereduces the risk of sensitization from 2% to 0.2%. If there is
any question regarding the need for prophylaxis, such as the certainty of
paternity, anti-D immune globulin should be administered. Some authorities
recommend that if delivery has not occurred within 12 weeks of the injection at
28 weeks of gestation, a second 300 μg dose of anti-D immune globulin should be
given.
Because
even a minute amount of fetal red cells can result in sensitization to the Rh D
antigen, in any circumstance when a fetomaternal hemorrhage can occur, a
prophylactic dose of 300 μg of anti-D immune globulin
should be administered.
Each dose of anti-D immune
globulin provides protection against sensitization for up to 30 mL of fetal
blood or 15 mL of fetal red blood cells.
In cases
of trauma or bleeding during pregnancy in which there is a potential for more
than a 30-mL fetomaternal trans-fusion, the extent of the fetomaternal
hemorrhage can be assessed using the Kleihauer-Betke test. This test
identifies fetalerythrocytes in the maternal circulation. The number of fetal
cells as a proportion of the total cells can be deter-mined and the volume of
fetomaternal hemorrhage can be estimated. Based on this estimation, the
appropriate dose of Rh immune globulin can be determined. An indirect Coombs
test can also be used to determine if the patient has received sufficient
antibody. A positive test indicates that she has received an adequate dose.
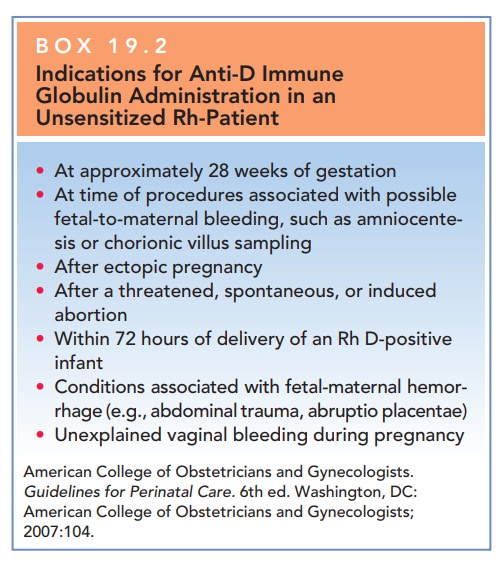
Box 19.2
Indications for Anti-D Immune Globulin Administration in an Unsensitized Rh-Patient
At approximately 28 weeks of gestation
At time of procedures associated with possible fetal-to-maternal bleeding, such as amniocente-sis or chorionic villus sampling
After ectopic pregnancy
After a threatened, spontaneous, or induced abortion
Within 72 hours of delivery of an Rh D-positive infant
Conditions associated with fetal-maternal hemor-rhage (e.g., abdominal trauma, abruptio placentae)
Unexplained vaginal bleeding during pregnancy
American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 6th ed. Washington, DC:American College of Obstetricians and Gynecologists; 2007:104.
Related Topics