Classification of Hypersensitivity | Immunology - Hypersensitivity | 12th Microbiology : Chapter 11 : Immunology
Chapter: 12th Microbiology : Chapter 11 : Immunology
Hypersensitivity
Hypersensitivity
Hypersensitivity
is defined as the exaggerated immunological response leading to severe symptoms
and even death in a sensitized individual when exposed for the second time. It
is commonly termed as allergy. The substances causing allergic/ hypersensitivity
is known as allergens. Example:. Drugs, food stuffs, infectious microorganisms,
blood transfusion and contact chemicals.
Classification of Hypersensitivity (Coombs and Gell Classification)
Type I: Immediate (Atopic or anaphylactic) Hypersensitivity
Type II:
Antibody–dependent Hypersensitivity
Type III:
Immune complex mediated Hypersensitivity
Type IV:
Cell mediated or delayed Hyper-sensitivity
Type I: Immediate (Atopic or anaphylactic) Hypersensitivity
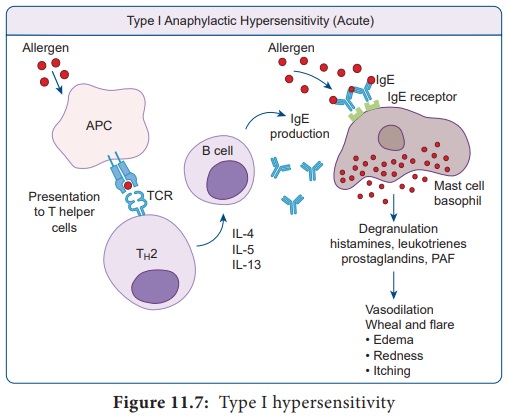
This type
of hypersensitivity is an allergic reaction provoked by the re-exposure to a
specific antigen. The antigen can make its entry through ingestion, inhalation,
injection or direct contact. The reaction may involve skin, eyes, nasopharynx
and gastrointestinal tract. The reaction is mediated by IgE antibodies (Figure
11.7). IgE has very high affinity for its receptor on mast cells and basophils.
Cross linking of IgE receptor is important in mast cell trigerring. Mast cell
degranulation is preceded by increased Ca++ influx. Basophils and
mast cells release pharmacologically active substances such as histamines and
tryptase. This causes inflammatory response. The response is immediate (within
seconds to minutes). Hence, it is termed as immediate hypersensitivity. The
reaction is either local or systemic.
Hay Fever
Allergic
rhinitis is commonly known as hay fever. Allergic rhinitis develops when the
body’s immune system becomes sensitized and overreacts to something in the
environment like pollen grains, strong odour of perfumes, dust etc. that
typically causes no problem in most people. When a sensitive person inhales an
allergen the body’s immune system may react with the symptoms such as sneezing, cough and puffy swollen eyelids.
Type II Hypersensitivity: Antibody dependent hypersensitivity
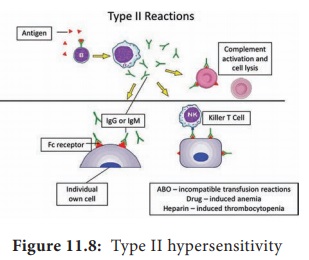
In this
type of hypersensitivity reactions the antibodies produced by the immune
response binds to antigens on the patient’s own cell surfaces. It is also known
as cytotoxic hypersensitivity and may affect variety of organs or tissues. Ig G
and Ig M antibodies bind to these antigens and form complexes. This inturn
activates the classical complement pathway and eliminates the cells presenting
the foreign antigen. The reaction takes hours to day (Figure 11.8).
Drug induced haemolytic anaemia
Certain drugs such as penicillin, cephalosporin and streptomycin can absorb non-specifically to protein on surface of RBC forming complex similar to hapten-carrier complex. In some patients these complex induce formation of antibodies, which binds to drugs on RBC and induce complement mediated lysis of RBC and thus produce progressive anaemia. This drug induced haemolytic anaemia is an example of Type II hypersensitivity reaction.
Type III Hypersensitivity: Immune complex mediated hypersensitivity
When a
huge amount of antigen enters into the body, the body produces higher
concentrations of antibodies. These antigens and antibodies combine together to
form insoluble complex called immune complex. These complexes are not
completely removed by macrophages. These get attached to minute capillaries of
tissues and organs such as kidneys, lung and skin (Figure 11.9). These antigen-
antibody complexes activate the classical complement pathway leading to
vasodilation. The complement proteins and antigen-antibody complexes attract
leucocytes to the area. The leukocytes discharge their killing agents and
promote massive inflammation. This can lead to tissue death and haemorrhage.
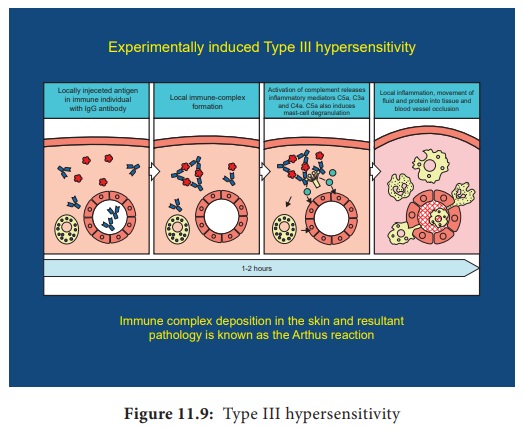
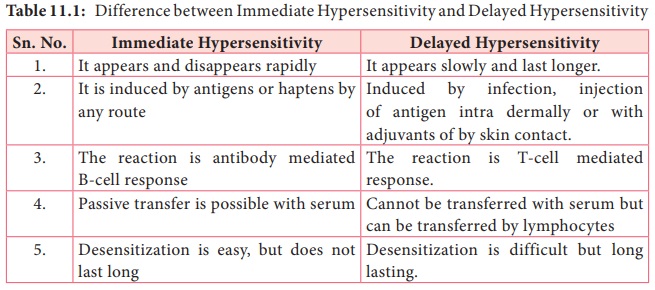
Arthus reaction
It was
first observed by Arthus. It is a local immune complex reaction occurring in
the skin. Horse serum and egg albumin are the antigens that induce the arthus
reaction. It is characterized by erythema, induration, oedema, haemorrhage and necrosis.
This reaction occurs when antibody is found in excess. It appears in 2–8 hours
after injection and persists for about 12–24 hours (Table 11.1)
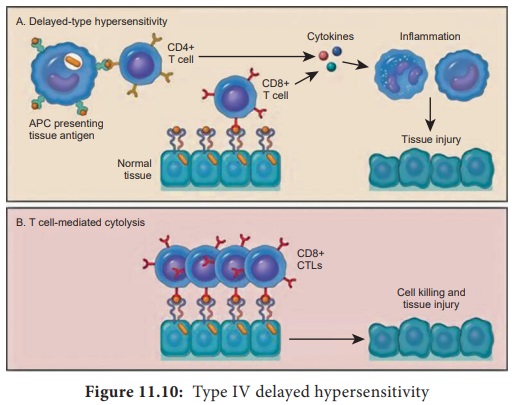
Type IV hypersensitivity: Cell Mediated Delayed Hypersensitivity
It is
often called as delayed hypersensitivity reaction as the reaction takes two to
three days to develop. Type IV hypersensitivity is involved in the pathogenesis
of many autoimmune and infectious diseases such as tuberculosis and leprosy. T
lymphocytes, monocytes and macrophages are involved in the reaction. Cytotoxic
T Cells cause direct damage whereas the T helper cells secrete cytokines and
activate monocytes and macrophages and cause the bulk damage (Figure 11.10).
Tuberculin reaction (Mantoux Reaction)
When a small dose of tuberculin is injected intra dermally in an individual already having tubercle bacilli, the reaction occurs. It is due to the interaction of sensitized T cell and tubercle bacterium. The reaction is manifested on the skin very late only after 48–72 hours.
Related Topics