Chapter: Essentials of Anatomy and Physiology: Human Development and Genetics
Human Development
HUMAN DEVELOPMENT
During the 40 weeks of gestation, the embryo-fetus is protected and nourished in the uterus of the mother. A human being begins life as one cell, a fertilized egg called a zygote, which develops into an individual human being consisting of billions of cells organized into the body systems with whose functions you are now quite familiar.
FERTILIZATION
Although millions of sperm are deposited in the vagina during sexual intercourse, only one will fertil-ize an ovum. As the sperm swim through the fluid of the uterus and fallopian tube, they undergo a final metabolic change, called capacitation. This change involves the acrosome, which becomes more fragile. When sperm and egg make contact, the acrosomal enzymes will digest the layers of cells and membrane around an ovum.
Once a sperm nucleus enters the ovum, changes in the egg cell membrane block the entry of other sperm. The nucleus of the ovum completes the second mei-otic division, and the nuclei of ovum and sperm fuse, restoring the diploid number of chromosomes in the zygote.
The human diploid number of 46 chromosomes is actually 23 pairs of chromosomes; 23 from the sperm and 23 from the egg. These 23 pairs consist of 22 pairs of autosomes (designated by the numerals 1 through 22) and one pair of sex chromosomes. Women have the sex chromosomes XX, and men have the sex chro-mosomes XY. Figure 21–1 shows the inheritance of gender. The Y chromosome has a gene that triggers the development of male gonads in the embryo. In the absence of the Y chromosome, the embryo will develop as a female.
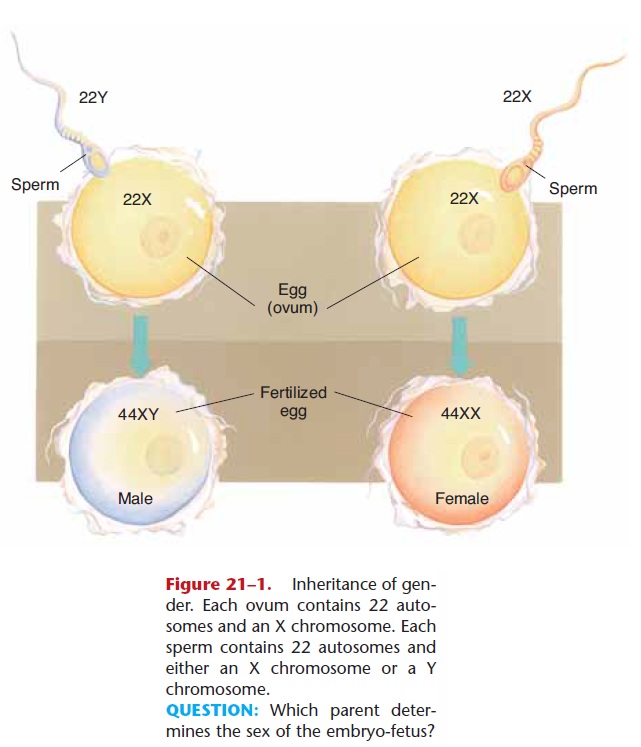
Figure 21–1. Inheritance of gen-der. Each ovum contains 22 auto-somes and an X chromosome. Each sperm contains 22 autosomes and either an X chromosome or a Y chromosome.
QUESTION: Which parent deter-mines the sex of the embryo-fetus?
IMPLANTATION
Fertilization usually takes place within the fallopian tube, and the zygote begins to divide even as it is being swept toward the uterus. These are mitotic divisions and are called cleavage. Refer to Fig. 21–2 as you read the following.
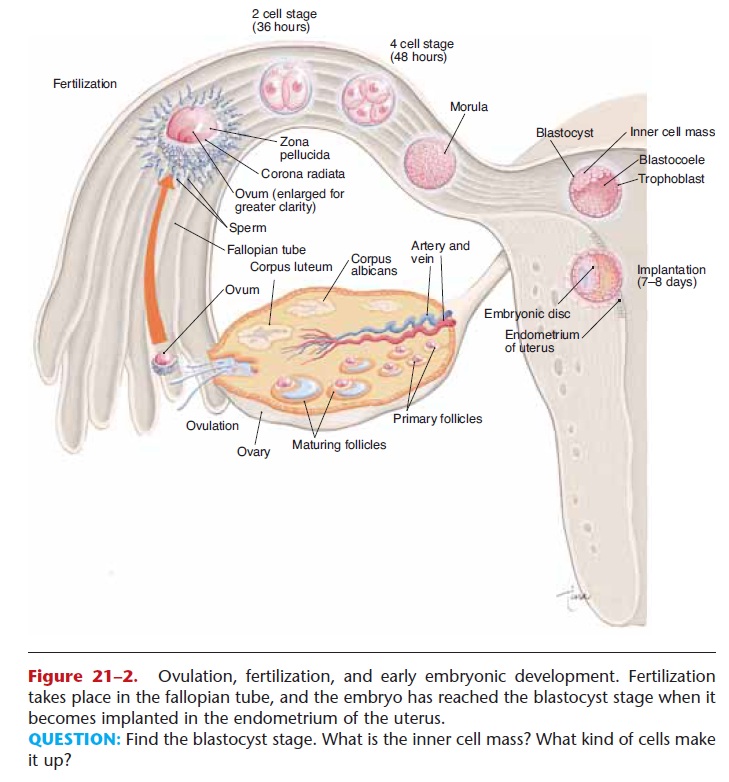
Figure 21–2. Ovulation, fertilization, and early embryonic development. Fertilization takes place in the fallopian tube, and the embryo has reached the blastocyst stage when it becomes implanted in the endometrium of the uterus.
QUESTION: Find the blastocyst stage. What is the inner cell mass? What kind of cells make it up?
The single-cell zygote divides into a two-cell stage, four-cell stage, eight-cell stage, and so on. Three days after fertilization there are 16 cells, which continue to divide to form a solid sphere of cells called a morula. As mitosis proceeds, this sphere becomes hollow and is called a blastocyst, which is still about the same size as the original zygote.
A fluid-filled blastocyst consists of an outer layer of cells called the trophoblast and an inner cell mass that contains the potential embryo. It is the blastocyst stage that becomes implanted in the uterine wall, about 5 to 8 days after fertilization.
Successful implantation is not simply a matter of the blastocyst contacting the uterine lining. The endo-metrium produces carbohydrate “docking” molecules toward the end of the uterine cycle, and the blastocyst has a surface protein that fits the docking sites. Once this “fit” is made, the trophoblast secretes enzymes to digest the surface of the endometrium, creating a small crater into which the blastocyst sinks. The trophoblast will become the chorion, the embryonic membrane that will form the fetal portion of the placenta. Following implantation, the inner cell mass will grow to become the embryo and other membranes.
The cells of the inner cell mass are embryonic stem cells. In these cells, all of the DNA has the potential for being switched on, that is, the potential exists for a cell to develop into any of the 200 kinds of human cells that will be present at birth. As the cells continue to divide and become more numerous, some DNA will be switched off in each cell, genes will become inactive, and the possibilities for the specialization of each cell will be narrowed down. The “switches” are chemicals, few of which are known at present. A great deal of research is focusing on discovering the stimuli that turn a stem cell into a muscle cell rather than a nerve cell or skin cell, and so on.
EMBRYO AND EMBRYONIC MEMBRANES
An embryo is the developing human individual from the time of implantation until the eighth week of ges-tation. Several stages of early embryonic development are shown in Fig. 21–3. At approximately 12 days, the embryonic disc (the potential person) is simply a plate of cells within the blastocyst. As cells keep divid-ing, the plate of cells begins to fold. At 14 days twin-ning is believed to be no longer possible.
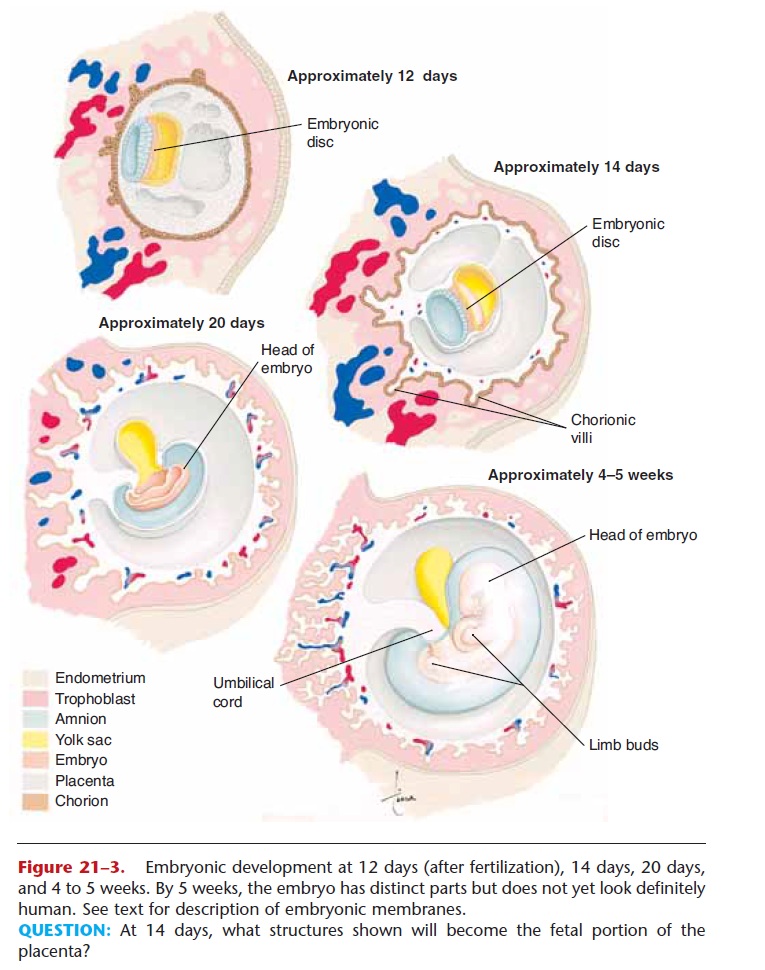
Figure 21–3. Embryonic development at 12 days (after fertilization), 14 days, 20 days, and 4 to 5 weeks. By 5 weeks, the embryo has distinct parts but does not yet look definitely human. See text for description of embryonic membranes.
QUESTION: At 14 days, what structures shown will become the fetal portion of the placenta?
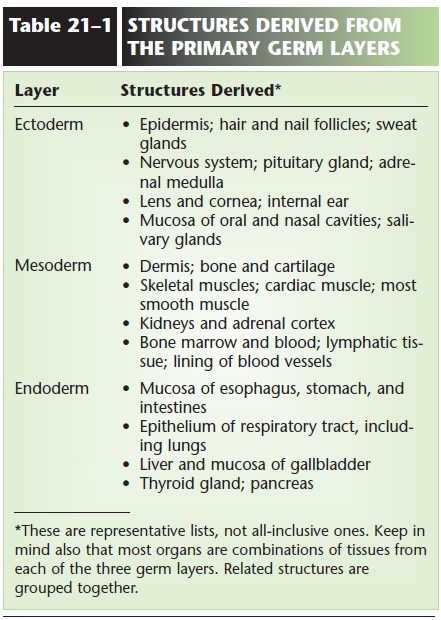
Very soon thereafter, three primary layers, or germ layers, begin to develop: the ectoderm, mesoderm, and endoderm. This is a major step in the specializa-tion of the embryo cells, because different sets of genes are switched off for each of the three layers, while the genes appropriate for the layer remain switched on. Each cell is now committed to a particu-lar layer and can no longer “go back,” that is, become a cell of either of the other two layers.
Each primary layer develops further; its cells become more specialized as more and more genes in each cell are switched off. With the active genes, those that remain switched on, the cells in each layer are thereby committed to develop into specific organs or parts of organs. Ecto means “outer”; the epidermis is derived from ectoderm, and in some of these cells the gene for producing keratin is active. Meso means “mid-dle”; the skeletal muscles develop from mesoderm, and in these cells the genes for producing myosin and actin are active. Endo means “inner”; the stomach lin-ing is derived from endoderm, and in these cells, the gene for producing pepsinogen is active. Table 21–1 lists some other structures derived from each of the primary germ layers.
At 20 days, the embryonic membranes can be clearly distinguished from the embryo itself. The yolk sac does not contain nutrient yolk, as it does for bird and reptile embryos. It is, however, the site for the for-mation of the first blood cells and the cells that will become spermatogonia or oogonia. As the embryo grows, the yolk sac membrane is incorporated into the umbilical cord.
The amnion is a thin membrane that eventually surrounds the embryo and contains amniotic fluid. This fluid provides a cushion for the fetus against mechanical injury as the mother moves. When the fetal kidneys become functional, they excrete urine into the amniotic fluid. Also in this fluid are cells that have sloughed off the fetus; this is clinically important
in the procedure called amniocentesis. The rupture of the amnion (some-times called the “bag of waters”) is usually an indica-tion that labor has begun.
The chorion is the name given to the trophoblast as it develops further. Once the embryo has become implanted in the uterus, small projections called chorionic villi begin to grow into the endometrium. These will contain the fetal blood vessels that become the fetal portion of the placenta.
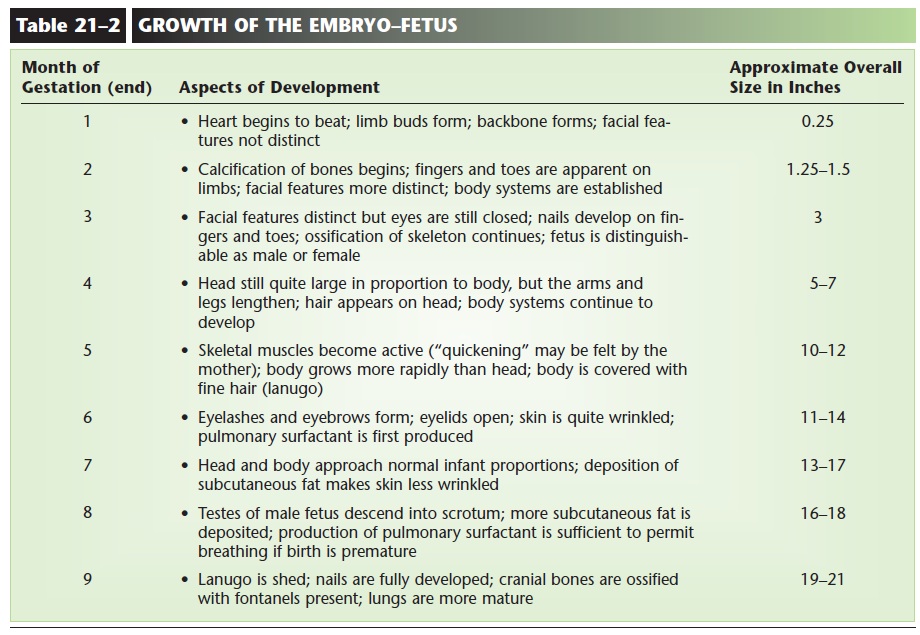
At about 4 to 5 weeks of development, the embryo shows definite form. The head is apparent, the heart is beating, and limb buds are visible. The period of embryonic growth continues until the 8th week. At this time, all of the organ systems have been estab-lished. They will continue to grow and mature until the end of gestation. The period of fetal growth extends from the 9th through the 40th week. Table 21–2 lists some of the major aspects of development in the growth of the embryo-fetus. The fetus at 16 weeks is depicted in Fig. 21–4. Maternal changes during pregnancy are summarized in Table 21–3.
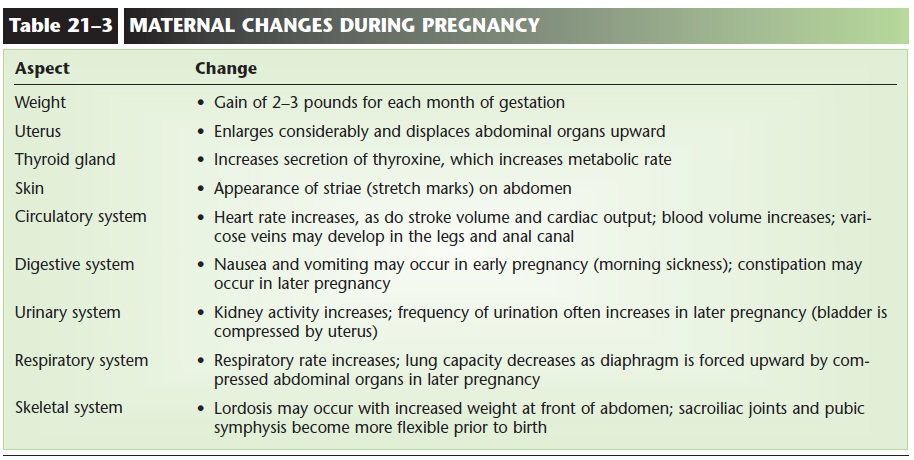
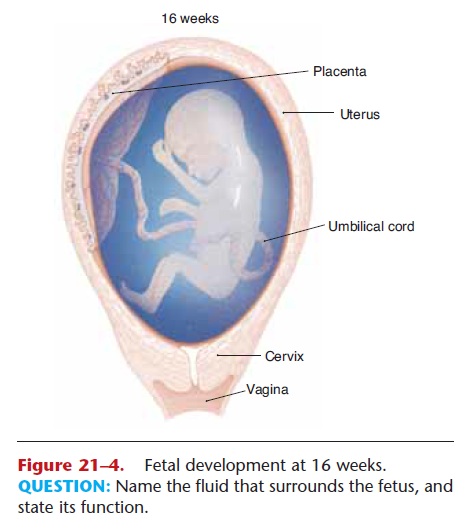
Figure 21–4. Fetal development at 16 weeks. QUESTION: Name the fluid that surrounds the fetus, and state its function.
PLACENTA AND UMBILICAL CORD
The placenta is made of both fetal and maternal tis-sue. The chorion of the embryo and the endometrium of the uterus contribute, and the placenta is formed by the third month of gestation (12 weeks). The mature placenta is a flat disc about 7 inches (17 cm) in diameter.
The structure of a small portion of the placenta is shown in Fig. 21–5. Notice that the fetal blood vessels are within maternal blood sinuses, but there is no direct connection between fetal and maternal vessels. Normally, the blood of the fetus does not mix with that of the mother. The placenta has two functions: to be the site of exchanges between maternal and fetal blood and to produce hormones to maintain preg-nancy. We will consider the exchanges first.
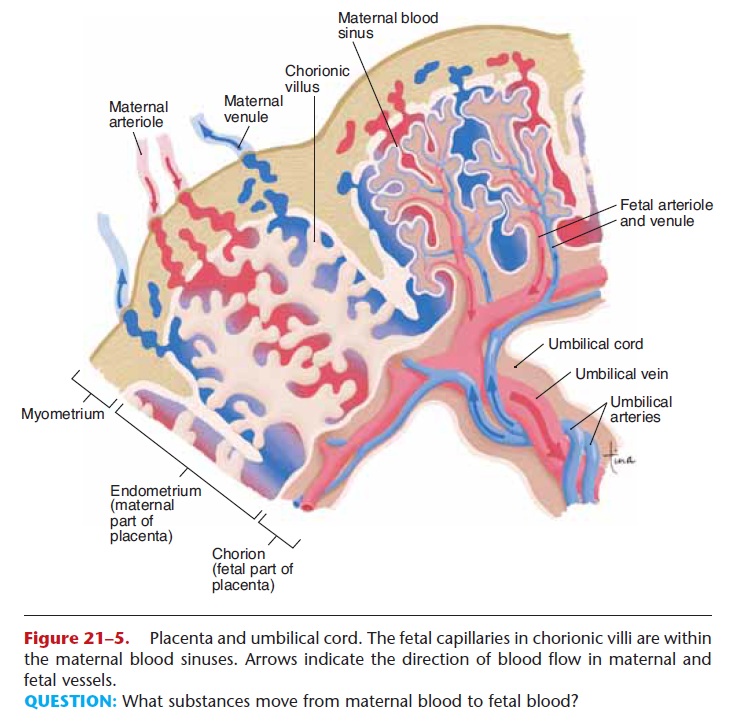
Figure 21–5. Placenta and umbilical cord. The fetal capillaries in chorionic villi are within the maternal blood sinuses. Arrows indicate the direction of blood flow in maternal and fetal vessels.
QUESTION: What substances move from maternal blood to fetal blood?
The fetus is dependent upon the mother for oxygen and nutrients and for the removal of waste products. The umbilical cord connects the fetus to the pla-centa. Within the cord are two umbilical arteries that carry blood from the fetus to the placenta and one umbilical vein that returns blood from the placenta to the fetus.
When blood in the umbilical arteries enters the placenta, CO2 and waste products in the fetal capillar-ies diffuse into the maternal blood sinuses. Oxygen diffuses from the maternal blood sinuses into the fetal capillaries; nutrients enter the fetal blood by diffusion and active transport mechanisms. This oxygen- and nutrient-rich blood then flows through the umbilical vein back to the fetus.
When the baby is delivered at the end of gestation, the umbilical cord is cut. The placenta then detaches from the uterine wall and is delivered, with the rest of the umbilical cord, as the afterbirth.
The blood in the remnant of the umbilical cord contains abundant stem cells, and their potential to become different kinds of cells is between that of embryonic stem cells (which may become any human cell) and adult stem cells (which are more limited). Umbilical cord stem cells have already been used to treat newborns with infantile Krabbe’s disease, a neu-rological disorder that is fatal by the age of 2 years. Such treatment depends on genetic testing and having suitable donated cord stem cells available at birth. Banks of cord blood are being established by some medical centers (because such donated blood can be frozen and stored), and the use of cord stem cells may someday decrease the need for bone marrow trans-plants.
Placental Hormones
The first hormone secreted by the placenta is human chorionic gonadotropin (hCG), which is produced by the chorion of the early embryo. The function of hCG is to stimulate the corpus luteum in the maternal ovary so that it will continue to secrete estrogen and progesterone.
The secretion of progesterone is partic-ularly important to prevent contractions of the myometrium, which would otherwise result in miscar-riage of the embryo. Once hCG enters maternal cir-culation, it is excreted in urine, which is the basis for many pregnancy tests. Tests for hCG in maternal blood are even more precise and can determine whether a pregnancy has occurred even before a men-strual period is missed.
The corpus luteum is a small structure, however, and cannot secrete sufficient amounts of estrogen and progesterone to maintain a full-term pregnancy. The placenta itself begins to secrete estrogen and proges-terone within a few weeks, and the levels of these hor-mones increase until birth. As the placenta takes over, the secretion of hCG decreases, and the corpus luteum becomes non-functional. During pregnancy, estrogen and progesterone inhibit the anterior pitu-itary secretion of FSH and LH, so no other ovarian follicles develop. These placental hormones also pre-pare the mammary glands for lactation.
The placenta also secretes relaxin, which helps inhibit contractions of the myometrium. Relaxin also permits stretching of the ligaments of the pubic sym-physis so that this joint will give a little, if necessary, during birth.
PARTURITION AND LABOR
Parturition is the rather formal term for birth, and labor is the sequence of events that occur during birth. The average gestation period is 40 weeks (280 days), with a range of 37 to 42 weeks.
Toward the end of gestation, the placental secretion of progesterone decreases while the estrogen level remains high, and the myometrium begins to contract weakly at irregular intervals. At this time the fetus is often oriented head down within the uterus (Fig. 21–6). Labor itself may be divided into three stages:
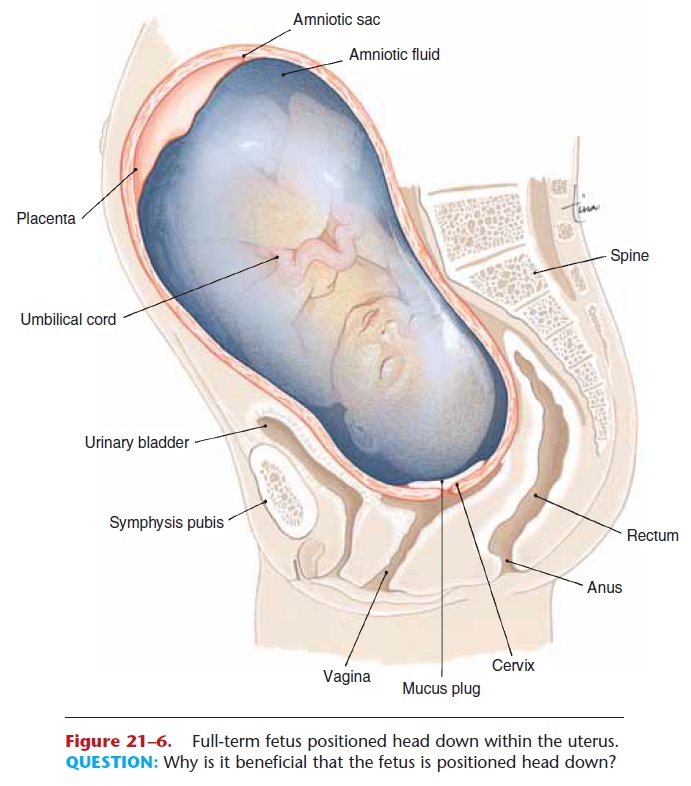
Figure 21–6. Full-term fetus positioned head down within the uterus. QUESTION: Why is it beneficial that the fetus is positioned head down?
First stage—dilation of the cervix. As the uterus con-tracts, the amniotic sac is forced into the cervix, which dilates (widens) the cervical opening. At the end of this stage, the amniotic sac breaks (rupture of the “bag of waters”) and the fluid leaves through the vagina, which may now be called the birth canal. This stage lasts an average of 8 to 12 hours but may vary considerably.
Second stage—delivery of the infant. More power-ful contractions of the uterus are brought about by oxytocin released by the posterior pituitary gland and perhaps by the placenta itself. This stage may be prolonged by several factors. If the fetus is positioned other than head down, delivery may be difficult.
This is called a breech birth and may necessitate a cesarean section (C-section), which is delivery of the fetus through a surgical incision in the abdominal wall and uterus. For some women, the central opening in the pelvic bone may be too small to permit a vaginal delivery. Fetal distress, as determined by fetal monitoring of heartbeat for example, may also require a cesarean section.
Third stage—delivery of the placenta (afterbirth). Continued contractions of the uterus expel the pla-centa and membranes, usually within 10 minutes after delivery of the infant. There is some bleeding at this time, but the uterus rapidly decreases in size, and the contractions compress the endometrium to close the ruptured blood vessels at the former site of the placenta. This is important to prevent severe maternal hemorrhage.
THE INFANT AT BIRTH
Immediately after delivery, the umbilical cord is clamped and cut, and the infant’s nose and mouth are aspirated to remove any fluid that might interfere with breathing. Now the infant is independent of the mother, and the most rapid changes occur in the respiratory and circulatory systems.
As the level of CO2 in the baby’s blood increases, the respiratory center in the medulla is stimulated and brings about inhalation to expand and inflate the lungs. Full expansion of the lungs may take up to 7 days following birth, and the infant’s respiratory rate may be very rapid at this time, as high as 40 respira-tions per minute.
Breathing promotes greater pulmonary circula-tion, and the increased amount of blood returning to the left atrium closes the flap of the foramen ovale. The ductus arteriosus begins to constrict, apparently in response to the higher blood oxygen level. Full closure of the ductus arteriosus may take up to 3 months.
The ductus venosus no longer receives blood from the umbilical vein and begins to constrict within a few minutes after birth. Within a few weeks the duc-tus venosus becomes a non-functional ligament.
The infant’s liver is not fully mature at birth and may be unable to excrete bilirubin efficiently. This may result in jaundice, which may occur in as many as half of all newborns. Such jaundice is not considered serious unless there is another possible cause, such as Rh incompatibility.
Related Topics