Chapter: Clinical Cases in Anesthesia : Asthma
How would you distinguish obstructive from restrictive lung disease, and asthma from chronic obstructive pulmonary disease (COPD)
How would you distinguish obstructive from
restric-tive lung disease, and asthma from chronic obstruc-tive pulmonary
disease (COPD), using preoperative pulmonary function tests?
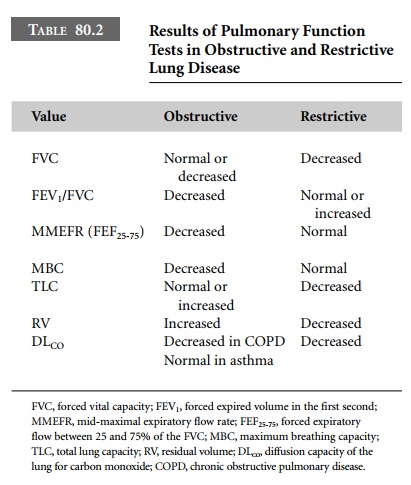
Pulmonary function tests (PFT) are comprised of
spirometry and flow-volume loops. An arterial blood gas and diffusion of carbon
monoxide (DLCO) can also be included. Typical values in obstructive
and restrictive lung disease are shown in Table 80.2.
Asthmatic patients usually have normal PFT
values between attacks and periods of exacerbation. Narrowing limited to the
small airways can yield a normal FEV1/FVC, but the FEF25-75
will be decreased. Bronchospasm may be triggered during PFT evaluation with
methacholine or histamine to assess airway reactivity in patients suspected of
asthma with normal baseline PFT values.
For patients with COPD, measurements are
repeated after inhaled bronchodilators to evaluate the degree of reversibility
or the spastic component, as opposed to the fixed component due to inflammation
and airway destruction.
FEV1/FVC is effort-dependent and
requires patient cooperation for accurate measurement, while FEF25-75
is effort-independent. It is obtained by dividing the volume expired between
75% and 25% of the FVC by the time elapsed between these two points.
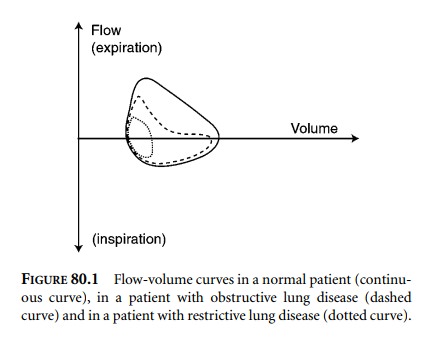
Flow-volume curves may also be helpful. A
normal curve as well as typical curves from patients with obstruc-tive and
restrictive disease are shown in Figure 80.1. By convention, inspiration is
below the baseline and expira-tion above. In restrictive disease, airway
resistance is normal with no flow limitation, while lung volumes are reduced.
In obstructive disease, the expiratory flow curve shows a characteristic flattening
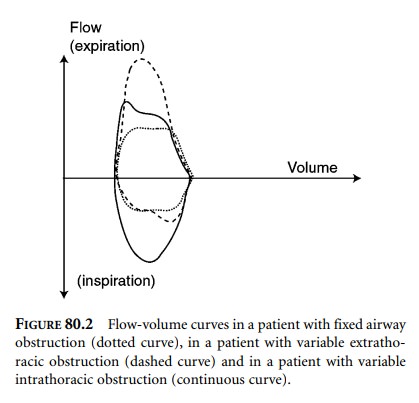
due to increased airway resistance. Curves from patients with fixed airway
obstruction and variable extrathoracic and intrathoracic obstructions are shown
in Figure 80.2. Fixed obstruction, such as is seen in tracheal stricture or
compression by a tumor or a goiter, causes a decrease in inspiratory and
expiratory flows. Variable extrathoracic obstruction (e.g., caused by vocal
cord paralysis or marked pharyngeal muscle weakness) causes collapse of the
airway during inspiration, as the transmural pressure gradient is negative. On
the other hand, with variable intrathoracic obstruction (e.g., caused by
tracheal or endobronchial tumor) the airway narrowing increases during forced
expiration.
Typically, the arterial blood gas (ABG) is
normal in asthmatic patients between attacks. Depending on the severity of the
attack, they will first show hypocapnia with normoxemia or mild hypoxemia. As
the attack becomes more severe, normocapnia then hypercapnia will be seen, with
worsening hypoxemia. The onset of hypercapnia is an ominous sign of impending
respiratory failure. In patients with COPD, the ABG shows a variable degree of
hypercapnia and hypoxemia. Patients with restrictive disease can have a normal
ABG at rest with hypercapnia and hypoxemia developing during exercise, or they
can have baseline abnormalities.
Related Topics