Chapter: Essential Anesthesia From Science to Practice : Clinical management : Pre operative evaluation
History - Clinical management
History
We begin with the “H” in “H&P,” obtaining a medical and surgical history. We are particularly concerned with the cardiopulmonary system, and exercise toler-ance is a good measure of current status. We also search for evidence of chronic diseases of other systems. For elective procedures, patients should be in the best condition possible, e.g., no exacerbation of chronic bronchitis or unstable angina. Below, we describe the pre-operative evaluation of some common medical condi-tions. When patients with these, or other rarer, conditions require an anesthetic, a pre-anesthesia clinic visit a week or so in advance of anesthesia allows time to seek additional information, e.g., study results from the patient’s private physi-cian, perform studies, e.g., cardiac pacemaker interrogation, or obtain consulta-tion from a specialist. Such planning helps keep the operating schedule running smoothly.
We
inquire about any previous anesthetics, particularly any untoward events such
as bleeding or airway difficulties. It is reassuring to learn a patient has
tol-erated previous anesthetics without difficulties. Next, we ask specifically
about any family history of anesthetic complications. A patient might not
realize that a remote event, such as his Aunt Edna dying with a raging fever
soon after an anesthetic many years ago, might mean that malignant hyperthermia
runs in his family. We need to ask specific questions to learn about inherited
con-ditions, including those related to plasma cholinesterase (see
Pharmacology: succinylcholine).
Medications
With
surprising frequency, review of the patient’s current medications reveals
previously unmentioned medical problems: “Oh, the digoxin? Well I don’t have a
heart condition now.” Many
medications influence the anesthetic, particularly those with cardiovascular or
coagulation-related effects. Some need to be dis-continued for some period
prior to surgery (see below), others must be converted from oral to parenteral
form to continue their effect. Many patients do not think of herbal compounds
when asked about their use of medicines and drugs. There-fore, we need to ask
specifically about herbals, some of which may present us with problems.1
Allergies
Common are patients with allergies to latex and to drugs. Questions about such sensitivities need to be asked of every patient lest we get confronted with a life-threatening anaphylaxis during anesthesia.
A distinction must be made, how-ever, between
sensitivities and true allergies. For example, a patient who “thought he was
going to die” in the dentist’s chair is probably not allergic to local
anes-thetics; rather, he likely had an intravascular injection, or rapid
absorption of epinephrine. Similarly, a patient who gets nauseated from codeine
can still receive fentanyl, which is chemically quite different from the
morphine-derived drugs. When an allergy is reported to a particular class of
drug, there are often other classes available to accomplish the same task. We
benefit our patients when we investigate these agents for potential
cross-reactivity. For example, a penicillin-allergic patient with a mild
reaction in childhood might receive a
cephalosporin safely (8% cross-reactivity); when determining the risk: benefit
ratio, you must take into consideration their reaction and the indication for
the cephalosporin.
Latex
allergy deserves special mention as its recognition has grown substan-tially in
recent years. The allergy to this natural rubber2
occurs after repeated exposure (as in the spina bifida patient who must
frequently catheterize his blad-der). Its sudden rise in healthcare workers
coincides with the 1980s admonition of “Universal Precautions” by the US
Occupational Safety and Health Adminis-tration – healthcare workers were
required to wear gloves to prevent transmission of AIDS and other viral
illnesses.
While
some patients merely note skin irritation from rubber gloves (probably not a
real allergy, but a precursor), of great concern is the patient who has
experi-enced throat swelling, for example when blowing up a balloon or painting
a room with latex paint. Latex is found in much of our medical equipment – from
breath-ing bags, to syringe plungers, to the puncturable tops on drug vials. In
a patient with latex allergy, we must eliminate all latex-containing products
from contact with the patient, including indirect contact such as drawing up
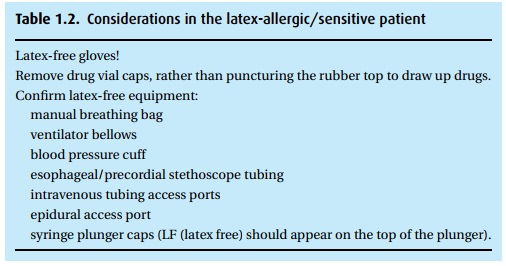
drugs through a latex plug (Table 1.2).
We
mentioned that healthcare workers are at risk. In fact, about one-third will
develop a contact dermatitis to latex gloves, while 10% or more may develop a
full-blown allergy, even more frequent in those who have other allergies, the
so-called atopic individual. We can reduce our risk of developing this allergy
by using non-latex gloves, or at least avoiding latex gloves containing
cornstarch. While the cornstarch makes the glove easier to don and remove, it
solubilizes the latex protein, increasing the chances of making its way through
the skin – par-ticularly through skin already irritated by the cornstarch; it
also helps the latex protein become aerosolized (and breathed in) upon glove
removal.
Habits
Moderate
tobacco and alcohol intake are not of great concern, but the chronic alcoholic
patient who has experienced delirium tremens, or the smoker who suf-fers severe
pulmonary disease confronts us with serious problems. Patients who take street
drugs also challenge us. On the one hand, they may not tell the truth about
their habits; on the other hand, if they do take drugs, their response to
anesthetics can be quite abnormal and troubling. These street drugs are known
by colorful names to some of their devotees. Anesthesia affects the respiratory
and cardiovascular systems; therefore, street drugs that depress the CNS can
exagger-ate respiratory depression, while CNS stimulants such a cocaine can
cause fatal cardiac complications.
Related Topics