Chapter: Essential Anesthesia From Science to Practice : Clinical management : Pre operative evaluation
Common disorders - Anesthesia Clinical management
Common disorders
We
encounter many patients with pre-existing medical conditions. Anesthetic and
operative procedures constitute a physiologic trespass with which the patient
can deal better, if not simultaneously challenged by correctable derangements
that sap his strength and threaten his homeostasis. Ideally, the surgeon would
already have addressed these questions. However, that is not always the case,
and the anesthesiologist needs to assess the medical condition of the patient.
The answers to the question, “Is the patient in the optimal condition to
pro-ceed with anesthesia and operation?” are not always clear-cut. For example,
a patient with transient ischemic attacks is scheduled for a carotid
endarterec-tomy. The patient also has coronary artery disease and unstable
angina. Should we risk the possibility of a stroke by first putting the patient
through a heart operation, or should we risk a myocardial infarction by first
doing a carotid endarterectomy? Consultations with other experts help in
resolving such difficult issues.
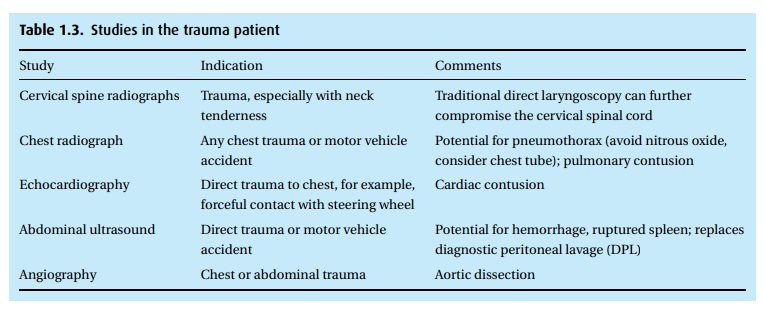
Trauma emergency
Rapid
assessment of the airway and fluid status precedes, or coincides with, the most
urgent: stemming of hemorrhage. Once we have secured an airway and established
a route for administering fluids, we can contemplate anesthe-sia, realizing
that a patient in hemorrhagic shock will tolerate and require very little
anesthesia. The mechanism of the trauma may suggest additional studies (Table 1.3).
Diabetes
We focus
on the many end-organ effects of diabetes, as well as the patient’s glu-cose control
(HgbA1c). Those with poor control should be considered for pre-admission.
Pre-operative studies should include assessment of metabolic, renal, and
cardiac status. In general, diabetic patients should be scheduled early in the
day.
Because
of the 30% incidence of gastroparesis in this population, diabetics are often
pretreated with metoclopramide to speed gastric emptying and are induced with a
‘rapid sequence induction’ (see General anesthesia). Intra-operative
man-agement aims to match insulin requirements, recognizing the fasting state
and the effects of surgical stress.
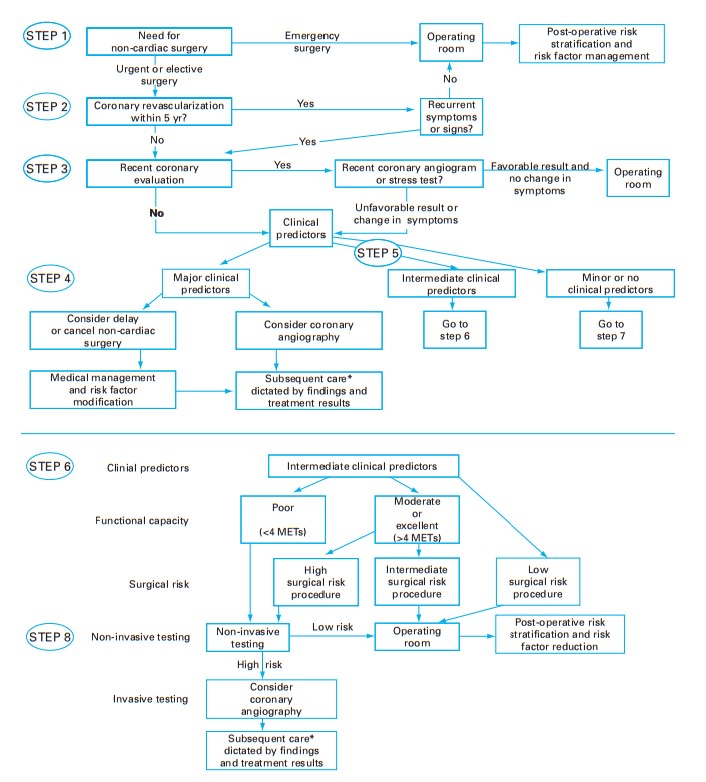
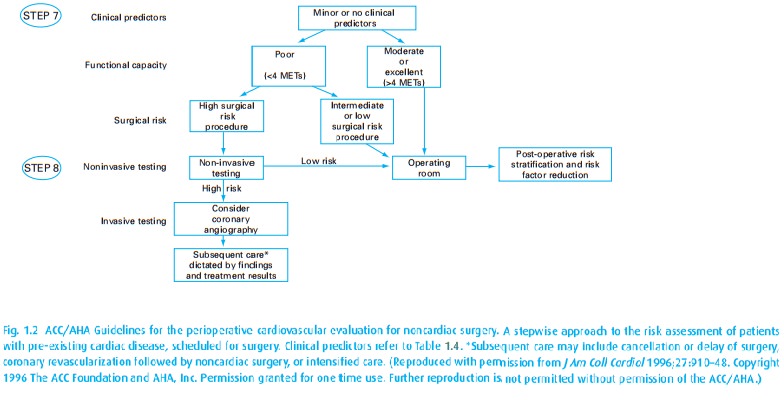
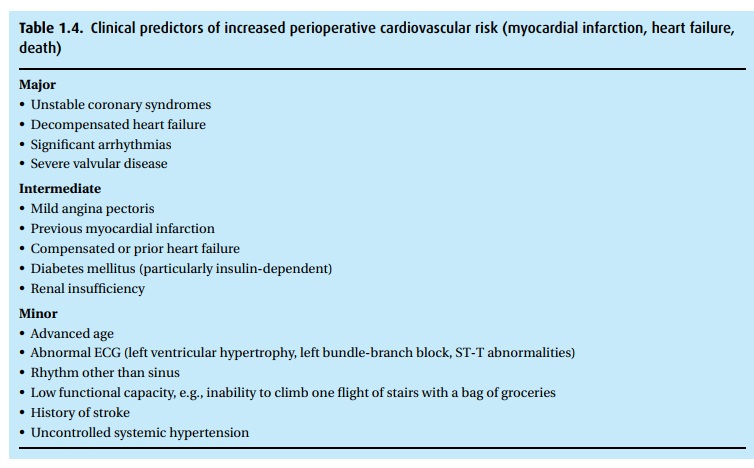
Coronary artery disease
In 2002,
the American College of Cardiology and the American Heart Association (ACC/AHA)
published updated guidelines for the perioperative cardiovascular evaluation of
patients for non-cardiac surgery. These so-called “Eagle criteria” should be
applied only when the results are likely to impact care. We should always ask
the patient about their exercise tolerance; the ACC/AHA recommendations attempt
to quantify this by using metabolic equivalents (METs), which enables us to
classify patients on a scale of 1 (take care of yourself around the house) to
10+ (participate in strenuous sports). A useful dividing line is 4
METs (climb a flight of stairs). In general, patients unable to do more than 4
METs represent a group at high risk of cardiovascular complications. The
algorithm in Fig. 1.2helps in assigning
risks and identifying those patients who require additional cardiac evaluation.
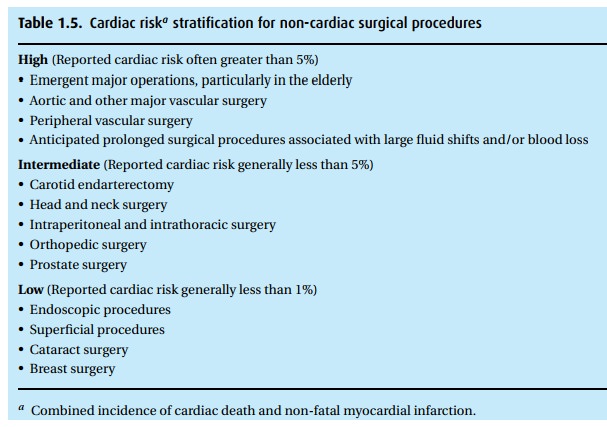
In addition to their functional capacity, the algorithm incorporates medical
status (Table 1.4) and the procedure planned
(Table 1.5).
Pacemaker/AICD
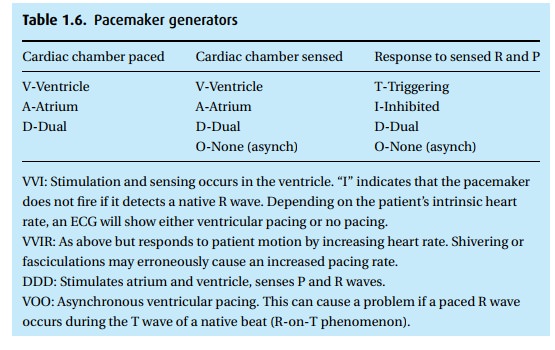
Pacemakers
are life saving for many patients with heart rhythm disturbances. There are
many types available, with a range of functionality (see Table 1.6). The addition of an automatic internal
cardiac defibrillator goes one step further. Unfortunately, these life-saving
devices may fail to function properly in the presence of electrical devices,
e.g., electrocautery. Many patients carry a card identifying the pacemaker make
and model. Some can also provide a report from a recent electronic
interrogation that specifies proper function and remain-ing battery life. More
often than not, we do not have that information. A chest radiograph can reveal
pacer make and model, as well as lead location. In symp-tomatic (lightheaded
spells, palpitations, hypotension) or in pacer-dependent patients, a pacemaker
interrogation (by a specialist with proprietary communi-cation equipment) may
be necessary. If this is not an option, a current ECG might be helpful, if it demonstrates pacer spikes in appropriate
locations.
Pulmonary disease
The
patient with pre-operative pulmonary disease faces risks of intra-operative and
post-operative pulmonary complications including pneumonia, bron-chospasm,
atelectasis, respiratory failure with prolonged mechanical ventilation, and
exacerbation of pre-existing lung disease. The risk of these complications
depends on both the patient and the procedure.
·
Chronic pulmonary disease Both chronic obstructive pulmonary disease(COPD)
and asthma can increase the risk. Therefore, well before anesthesia and surgery
we should treat the patient to bring him into the best possible condition,
given his lung disease.
·
Smoking Even without evident lung disease, smoking
increases the risk of pul-monary complications up to four times over that or
non-smokers. Eight weeks of smoking cessation isf required to reduce that risk,
though carboxyhemoglobin will virtually vanish after only 24 smoke-free hours.
·
General health There are general risk indices that predict
pulmonary compli-cations well. In fact, exercise tolerance alone is an
excellent predictor of post-operative pulmonary complications.
·
Obesity Obese patients present more airway management
difficulties for severalreasons: (i) mechanical issues related to optimal
positioning; (ii) redundant pharyngeal tissue complicating laryngoscopy; (iii)
many suffer from obstructive sleep apnea (and its sequelae: pulmonary
hypertension/cor pulmonale); and (iv) in obese patients it can be extremely difficult
or impossible to mask–ventilate the lungs due to the weight of the chest wall.
Obesity also increases the risk for thromboembolic phenomena. Post-operatively,
however, obesity has not proven to increase the risk of pulmonary
complications.
·
Surgical site Proximity of the surgical site to the diaphragm
is the single mostimportant predictor of pulmonary complications. Thoracic and
upper abdom-inal operative sites confer a 10–40% incidence. This can be reduced
perhaps 100-fold with laparoscopic techniques.
·
Surgery duration Operations lasting<3 hours are associated with fewercomplications.
·
Intra-operative muscle relaxants Pancuronium, specifically, has been
associatedwith an increased incidence of pulmonary complications; this is
related to its long half-life and risk of residual muscle weakness.
·
Results of pre-operative testing Routine pre-operative pulmonary function
tests(PFTs) are not indicated, unless the patient is undergoing lung resection.
If available, however, the risk of complications increases when the forced
expira-tory volume in 1s (FEV1) or forced vital capacity (FVC) are <70% predicted, or when the FEV1/FVC
is <65%
Asthma
Pre-operatively,
our goals are to reverse bronchospasm and inflammation, pre-vent an asthma
exacerbation, clear secretions, and treat any infection. We specif-ically ask
about any increased inhaler use, recent hospitalizations or Emergency
Department visits for bronchospasm, a recent change in sputum amount or color,
or a recent cold. All of these factors increase the risk of peri-operative
bron-chospasm. If the patient is scheduled for thoracic or upper abdominal
surgery (with a very high risk of pulmonary complications), spirometry can
identify patients at greatest risk.
Glucocorticoids
may be helpful in those patients who do not respond ade-quately to 2
agonists. Patients who are steroid dependent will often have suppressed adrenal
cortical function and require supplemental steroids in the peri-operative
period.
Chronic renal failure
Chronic
renal failure (CRF) involves both the excretory and synthetic functions of the
kidney. When the kidney fails to regulate fluids and electrolytes, the net
result is acidosis, hyperkalemia, hypertension, and edema. Meanwhile, the lack
of syn-thetic function results in anemia (due to decreased production of
erythropoietin) and hypocalcemia from a lack of active vitamin D3
(this also leads to secondary hyperparathyroidism, hyperphosphatemia, and renal
osteodystrophy). Azotemia can cause platelet dysfunction.
Medications
that are renally excreted will be affected by CRF, and most should be avoided.
In particular, meperidine (pethidine, Demerol®) should not be given as its
metabolite (normeperidine) can accumulate and cause seizures. The pre-ferred
muscle relaxant is one that does not depend on renal function for its
metabolism (atracurium, cis-atracurium
for surgical relaxation).
We check
electrolytes on these patients pre-operatively and prefer they undergo dialysis
within the preceding 24 hours. We must resist the temptation to hydrate a patient
who is intravascularly ‘dry’ following dialysis, as they cannot excrete excess
fluids. Replacement fluids should not contain potassium (normal saline is
preferred over Ringer’s lactate) as these patients are at risk for
hyperkalemia. CRF patients are also at increased risk for coronary artery and
peripheral vascular disease.
Related Topics