Chapter: 12th Nursing : Chapter 7 : Midwifery Nursing
High Risk Pregnancy
High Risk Pregnancy
Definition
High Risk Pregnancy is a pregnancy complicated by a disease or a disorder
that may endanger the life or affect the health of the mother, the fetus or the
newborn
Maternal Death Incidence
A maternal death is death of a Woman while pregnant or within 42
days of termination of pregnancy irrespective of the duration and the site of
the pregnancy, from any course related to or aggravated by the pregnancy or in
management but not from accidental or incidental causes. - WHO
·
20-25% deaths occur
during pregnancy.
·
40-50% deaths occur
during labour and delivery.
·
25-40% deaths occur
after childbirth (More during the first seven days)
·
Annually, 585,000 women
die of pregnancy related complications
High risk mothers are
·
Women below 18 years,
over 35 years in primigravida
·
Women who had four or
more pregnancies
·
Short Structure (height
<145 cm and below)
·
Twins
·
Aneamia
·
Previous Abortion, Intra
uterine death.
·
Malnutrition mother.
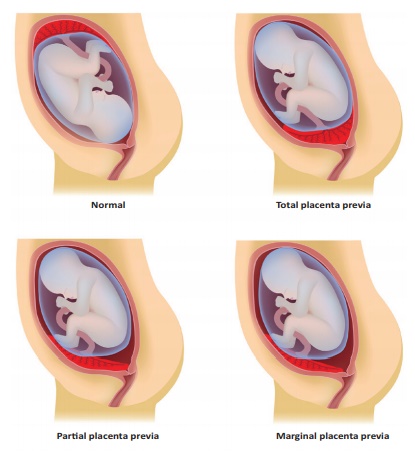
1. Placenta Praevia
DEFINITION: Placenta Praevia is a condition where the placenta is
implanted completely or partially in the lower part of the uterus.
Cause: Unknown
Risk factors: Multiparity, multiple gestations, previous uterine surgery
Manifestations: Painless, bright red bleeding >
20th week; episodic,
starts without warning, stops & starts again.
Vaginal examination is contra - indicated.
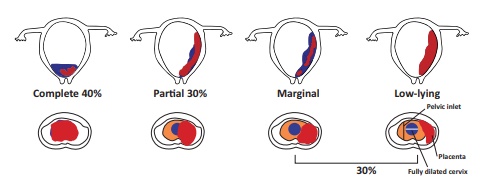
Types of Placenta Praevia
·
First degree (Type I):
Low lying Placenta the lower edge of the placenta reaches the lower uterine
segment but not the internal cervical os.
·
Second degree (Type II):
Marginal the lower edge of the placenta reaches the margin of the internal os
but does not cover it.
·
Third degree (Type III):
Incomplete or partial the placenta covers the internal os partially.
·
Fourth degree (Type IV):
Total placenta covers the internal os completely.
Management
Management depends upon gestational age, amount of bleeding and
fetal condition.
·
Monitor Fetal Heart
Rate, maternal Vital signs
·
Intra Venus Fluid
administration
·
O2 administration
·
Assess intake and
output, amount of bleeding
·
Do complete Blood count
and Rh factor test (CBC), Type and cross match for transfusion.
·
Ultrasound
·
No pelvic exams
·
No vaginal delivery- may
lead to haemorrhage
·
Prepare for caesarean
section
Prognosis: depends on amount of bleeding & gestational age
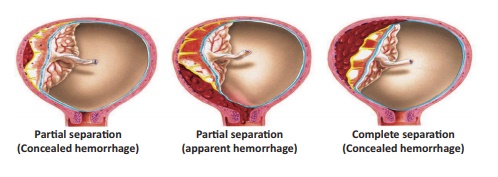
2. Abruptio Placenta
Abruptio Placenta: Premature separation of normally situated
placenta.
Cause: Unknown
Types of Abruptio placenta:
Concealed - The blood collects behind the separated placenta or
collected in between the membranes and decidua. (Blood is not visible outside)
Rare type.
Revealed - Following separation of the placenta, the
blood comes out of the cervical canal to be visible externally (commenest type)
Risk factors
·
Smoking
·
Short umbilical cord
·
Advanced maternal age
·
HTN
·
PIH
·
Cocaine use
·
Trauma to or near
abdomen.
Manifestations: Tenderness mild to severe constant pain;
mild to moderate bleeding depending on degree of separation.
Management
·
Monitor Fetal Heart
Rate, maternal Vital signs
·
Intra Venous Fluid
administration
·
O2 administration
·
Assess intake and
output, amount of bleeding
·
Do complete Blood count
and RH factor test (CBC), Type and cross match for transfusion.
·
Ultrasound
·
No pelvic exams
·
No vaginal delivery- may
lead to haemorrhage
·
Prepare for caesarean
section
3. Amniotic Fluid
DEFINITION: Amniotic fluid is a clear, slightly yellowish liquids
surround and protects the fetus during pregnancy. Normal Amniotic fluid is
around 800 ml
Amniotic fluid is made up of fetal urine & fluid
that is transported through placenta from maternal circulation.
Polyhydramnios
Polyhydramnios is defined as a state where amniotic fluid exceeds
more than 2000 ml.
Risk factors
·
Multiple pregnancy.
·
Fetal abnormalities.
·
Fetal skeletal
malformations.
·
Obstruction of GI tract-
prevents normal ingestion of amniotic fluid.
·
Rh Iso immunization
·
Maternal Diabetes
Mellitus.
·
Spinabifida;
Anencephaly, Hydrocephaly. Diagnosis: Sonography-To detect Amniotic Fluid
Index (AFI) is more than 20 cm. (Normal AFI is 8-18 cm).
Management
·
Bed rest.
·
Monitor weight gain.
·
Remove excess amniotic
fluid every 1-2 weeks through amniocentesis.
·
Most women with mild
polyhydramnios deliver healthy baby.
Oligohydramnios
It is a condition where the amniotic fluid is less than 500 ml in
the amniotic sac.
Causes
·
Failure of fetal kidney
development
·
Obstruction in urinary
tract
·
Intra Uterine Growth
Restriction (IUGR)
·
Post-term pregnancy
·
Premature rupture of
membrane
·
Fetal anomalies
·
Poor placental function.
Diagnosis
·
AFI < 5-6 cm
·
Small uterine size.
·
Less fetal movements
·
Prominent fetal parts on
palpations
·
Small for date uterine
size.
·
Fetal demise.
·
Ultrasonogram
Prognosis: Depends on severity of disease.
Management
·
Careful assessment of
mother/fetus
·
Frequent ante-partum
testing
·
Determine optimal time
for delivery (early)
·
Antibiotics/corticosteroids
with PROM (Premature Rupture Of Membranes)
4. Ectopic Pregnancy
The fertilized ovum is implanted and develops outside the normal
uterine cavity usually in fallopian tubes, rare on ovary, cervix or abdominal
cavity.
Incidence
·
Leading cause of death
from hemorrhage in pregnancy
·
Reduces fertility
·
1 in 100 pregnancies
Causes
·
Scarring of fallopian
tubes (Chlamydia/ Gonorrhea).
·
More common with
infection of fallopian tubes or surgery to reverse Tubale Ligation.
·
Previous ectopic
·
Multiple induced
abortions
·
Diethylstilbestrol (DES)
exposure
Symptoms
·
Colicky, cramping pain
in lower abdomen on affected side
·
Tubal rupture:
sudden/sharp/steady pain before diffusing throughout pelvic region
·
Heavy bleeding causes
shoulder pain, rectal pressure
·
Dizziness/weakness - If
tube ruptures, weak pulse, clammy skin, fainting. Assess for s/s shock.
Diagnosis
Estimation of Beta hCG (more than 1500 IU/L
·
Ultrasonogram
Treatment
·
Immediate surgery to
remove/repair tube.
·
If no rupture,
Methotrexate - stops cellular division in fetus; causes cell death. Conceptus
expelled with bleeding.
5. Hypertension In Pregnancy
Global cause of maternal/fetal morbidity mortality. Responsible
for 76,000 deaths/ year. Normotensive patient may become hypertensive in late
pregnancy, during labor, or 24 hours postpartum.
Pre-Eclampsia
Defined As
Pre-Eclamsia is characterised by hyper tention protrinuria and
oedema.
Dangers of Pregnancy Induced Hyper tention (PIH)
·
BP ≥ 140/90 mmHg
·
Systolic ↑
of 30mm Hg > pre-pregnancy. levels
·
Diastolic ↑
of 15mm Hg > pre pregnancy. levels.
·
Presents with HTN
(Hypertension), proteinuria, edema of face, hands, ankles.
·
Can occur anytime >
20th week of pregnancy.
·
Usually occurs closer to
due date. Will not resolve until birth.
General Signs of PRE-ECLAMPSIA
·
Rapid weight gain;
swelling of arms/face
·
Headache; vision changes
(blurred vision, seeing double, seeing spots)
·
Dizziness/faintness/ringing
in ears/ confusion; seizures
·
Abdominal pain, ↓
production of urine; nausea, vomiting.
·
Alarming signs:
U - Urinary output dimished S - Sleep disturbance
H - Headache
E - Epigastric pain and eye symptoms.
Eclampsia
Seizures or coma due to hypertensive encephalopathy
Incidence
·
Most serious
complication.
·
Affects ~ 0.2%
pregnancy.
·
Major cause of maternal
death due to intracranial hemorrhage.
·
Maternal mortality rate
is 8-36%.
Risk factors
·
< Age 20 years or
> 40 years
·
Twins, triplets
·
Primigravida
·
Molar pregnancy
·
Preexisting HTN,
Diabetes mellitus
·
Renal or vascular
disease
·
Previous history of
preeclampsia/eclampsia Causes: Unknown.
Management: Usually only cure is termination of pregnancy. It depends
upon symptoms.
Mild preeclampsia
·
Bedrest
·
Monitor at home or
hospital.
·
Deliver close to EDD
·
Frequent Blood Pressure,
24 hours urine, liver enzymes
·
Fetal Heart Rate
·
Ultrasounds.
Severe preeclampsia: BP = 160/110 mmHg, epigastric pain, 2-4+
proteinuria, ^ liver enzymes, thrombocytopenia [↓ 100,000].
Goal: prevent convulsions & control BP. Magnesium sulphate is
the drug of choice
Magnesium Toxicity based on clinical signs: such as sharp
drop in BP, respiratory paralysis and disappearance of patellar reflex.
·
STOP infusion
·
O2 administration
·
Calcium gluconate if
magnesium sulphate toxicity present
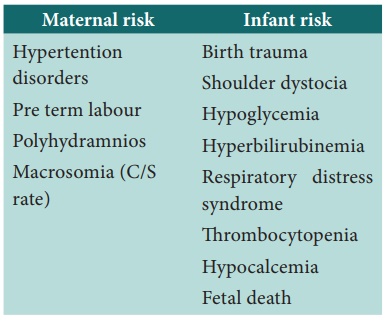
6. Gestational Diabetes Mellitus
Glucose intolerance beginning in pregnancy.ussually present in the
second or during the third trimester. Fasting blood sugar exceeds 90 mg/dl and
post prandial value is greater than 120 mg/dl
Pathophysiology
Pregnancy hormones estrogen, HPL, prolactin, cortisol,
progesterone, blocks insulin receptors > 20 weeks pregnancy.
·
Results in increased
circulating glucose
·
More insulin released to
attempt to maintain glucose homeostasis
·
Patient feels “hungry”
due to increased insulin
·
vicious cycle of
increased appetite & weight gain results
Diagnosis
·
Oral Glucose Challenge
Test (OGCT)
·
Screen all women at
24-28 weeks.
·
HIGHER Risk patient to
be screened in 1st trimester/1st prenatal visit and at 24-28 weeks.
Determining High Risk Clients
·
Family history DM;
Previous GDM
·
Marked obesity;
Glycosuria
·
Maternal Age > 30
·
Previous infant >
4000g
·
Member of high-risk
racial/ethnic group
·
Hispanic, Native
American, South or East Asian, African American, Pacific Islander.
·
If results negative,
repeat during 24-28wks.
Interventions
Antepartum Goal: strict glucose control.
·
Provide immediate
education to patient. and family members
·
Standard diabetic diet
[2000-2500 cal/day].
·
Total calories –
30Kcal/Kg for normal weight women
Distribution of calories: 40-50% carbs, 20% protein, 30-40% fat,
Recommend: 3 meals & 3 snacks evenly spaced to avoid swings in
blood glucose. Snack at bedtime.1200 mg/day calcium, 30 mg/day iron, 400
mcg/day folate.
Intrapartum: monitor glucose levels and titrate with insulin
Postpartum: Mostly return to normal after delivery.
·
50% patients. with GDM
develop type II later in life.
·
After 6 wk. PP (Postprandial)
serum glucose estimation to be done
·
Children of GDM
(Gestational Diabetes Mellitus) patients. ^ risk for obesity/ diabetes in
childhood/adolescence
Pre-Conception Planning:
·
Begin during
reproductive years
·
Maintain normal HbA1c
3-6 months before conception & during organogenesis (6-8weeks) –minimize
risk of spontaneous AB & congenital anomalies.
·
HbA1c level > 7:
increased risk for congenital anomalies & miscarriage. (Normal HbA1c = 4-6
%. )
·
Multidisciplinary team:
nutritionist, endocrinologist, high risk OBG nurse.
·
Educate patient.-
managing diet, activity, insulin Excercise
Daily food diary to assess compliance.
Related Topics