Chapter: 12th Nursing : Chapter 7 : Midwifery Nursing
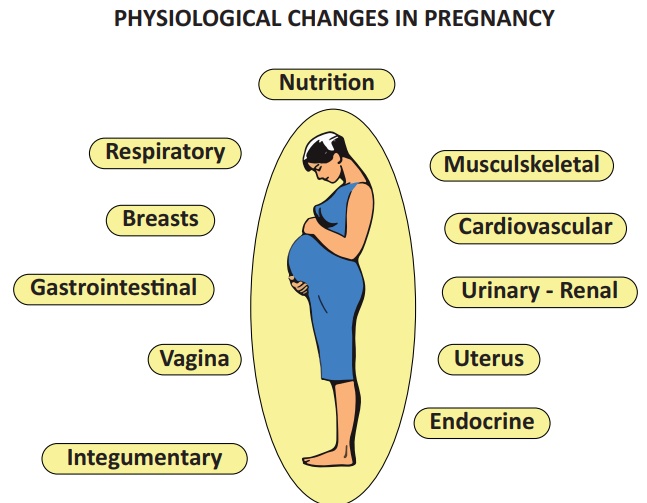
Diagnosis of Pregnancy
Diagnosis of Pregnancy
First Trimester
Presumptive signs:
·
Amenorrhoea-Absence of
menstruation.
·
Morning sickness-
Nausea, vomiting on rising from bed, loss of appetite.
·
Frequency of micturition
due to congestion of the bladder mucosa.
·
Breast discomfort-
feeling of fullness and ‘Pricking sensation’ is present.
·
Darkening of the
nipples, primary and secondary areolar change.
·
Fatigue or tiredness.
Probable signs
·
Breast changes: The
breasts are enlarged, evident between 6 to 8 weeks.
·
Vaginal Sign- The walls
become softened and looks bluish in colour. Copious non irritating mucoid
discharge appears at 6th week.
·
Osiander’s sign- There
is increased pulsation, felt through the laternal fornices at 8th week.
·
Jacquemier’s or
Chadwick’s sign - a bluish discoloration of the cervix, vagina and labia. This
is due to local vascular congestion.
·
Hegar’s Sign- Upper part
of the uterus is enlarged by the growing fetus, and lower part of the body of
the uterus is empty and extremely soft.
Positive signs
·
Fetal heart sounds.
·
Fetal movements.
·
Fetal parts.
Diagnostic test:
·
Blood/urine test for
Beta HCG (Human Chorionic Gonadotropin)
·
Ultrasonogram
Second Trimester (13-28 Weeks)
·
Quickening(feeling of
life): The perception of active fetal movement by the woman. Usually felt
during 18-20 weeks of pregnancy.
·
Progressive enlargement
of the lower abdomen by a mass(fetus)
·
chloasma-Pigmenation
over the forehead and cheek, appear at 24th week.
·
Braxton-Hicks
contraction: Braxton-Hicks contraction-Irregular, Infrequent, spasmodic
painless uterine contraction without any effect on dilation of cervix.
·
Ballottment of the
uterus.
·
Fetal heart sound (FHS)
is elicited around 20th weeks by fetoscope with doppler by 16th weeks.
Third Trimester (29-40 Weeks)
Symptoms
·
Amenorrhea continues
·
Enlargement of the
abdomen
·
Lightening(fetal head
sink in to the pelvic brim)
·
Frequency of micturition
Signs
·
Skin changes are more
prominent
·
Uterine shape is changed
from cylindrical to spherical
·
Fundal height up to the
level of ensiform cartilage
·
Braxton Hicks
contraction
·
Fetal movement are
easily felt.
·
Fetal parts are
Palpable.
·
Fetal heart rate
Calculation of Expected Date of Delivery [EDD]
EDD is calculated from first day of the Last Menstural Period
[LMP] by using Naegle’s formula. For calculation, 9 calendar months and 7 days
are added in the LMP
Gestational age – It is to be calculated as completed
weeks of gestation
1. Antenatal Care
Antenatal care refers to the care given to an expectant mother
from the time of conception to the beginning of labour. It includes,
·
Maternal health check
ups.
·
Evaluation of fetal
health and development
·
Detection of high risk
pregnancies e.g
GDM, PIH
·
Prompt intervention to
prevent complications.
·
Health education. e.g
Diet, exercise and follow up
Aims
·
To achieve a healthy
mother and baby.
·
To provide psychological
support to the women and her family.
·
To educate the women
regarding health care during pregnancy.
·
To monitor progress of
pregnancy and the baby.
·
To recognize deviation
from the normal and provide treatment as required.
·
To prepare women
physically and emotionally for the child birth, lactation and care of the baby.
·
To prevent congenital
deformities by educating the mother to avoid smoking, substance abuse and self
medications.
Antenatal Visits
Routine prenatal visits has been followed as convention and not an
evidence based benefits.
·
Initial visits at early
pregnancy (when a women missed her first period.
·
Every 4 weeks until 28
weeks
·
Every 2 weeks until 36
weeks
·
Every week until delivery
Antenatal visits should cover the following
·
History collection
·
Examination
·
Investigation
History Collection
a) Socio economic status
Low socio-economic status increases the risk of perinatal
morbidity and mortality.
b) Age
Maternal age younger than 20 years increases the risk of premature
births, late prenatal care, low birth weight, uterine dysfunction, fetal death,
neonatal death
Maternal age older than 35 years increases the risk of first
trimester miscarriage, genetically abnormal fetus, medical complication
(Hypertension, Diabetes, Eclampsia), multiple gestation, fetal morbidity and
mortality.
c) Menstrual history
• Age of menarche
• Cycle : regular/irregular
• Amount and duration of blood flow
• LMP- date is counted from the first day of the last menstrual
period
• EDD- calculate from LMP
d) Contraceptive history
Use of contraceptives copper T, or oral pills.
e) Past obstetric history
• Previous miscarriage
• Previous viable pregnancies
• Still births or neonatal deaths
• Method of delivery
• Gestational age, sex and weight of infants
• Previous antenatal or postnatal complications
d)
Previous
medical history
• Diabetes
• Cardiac diseases
• Hypertension
• Renal diseases
·
Infectious diseases such
as HIV, Hepatitis B or C
e) Personal history
• Smoking
• Alcohol
• Substance abuse
f) Family history
·
Diabetes
·
Hypertension
·
Tuberculosis
·
Twins
Examination
General state of health:
·
Build - obese, average,
thin
·
Nutritional status -
good, average, poor
·
Gait - normal, with a
limp,
·
Postures - Kyphosis,
Scoliosis, Lordosis
·
Personal hygiene
Height – A short stature women (<145cm) may have a small pelvis
leading to difficulty in labour.
Weight - Monitor for weight gain regularly
·
Inadequate weight gain
may indicate low birth weight baby,Intra Uterine Growth Retardation( IUGR )and
poor perinatal outcome.
·
Excessive weight gain
may be due to fluid retention, pre-eclampsia, multiple pregnancies, polyhydramnios.
Pallor – It is a indicative of anemia, examine conjunctiva, tongue
and nails for pallor.
Jaundice – Yellowish discoloration of the sclera, palate and skin.
Oedema – Examine for pitting oedema over the legs above the medial
malleolus.
Breast and nipple – Observe the skin changes over the
breast, gently palpate the breast for any tumor or nodule, look for any crack
or retracted nipple.
Teeth and gums – women with dental carries, gingivitis
or poor oral hygiene should be reported.
Varicosities – Note the presence of varicose vein and their
distribution.
Vital signs – Record pulse, respiration, temperature and blood pressure
and report any abnormality.
Abdominal Examination should be performed in each visit.
Steps of Abdominal Examination:
·
Inspection
·
Palpation
Auscultation
Inspection
·
Abdomen
·
Size
·
shape
·
Contour – spherical,
cylindrical, pendulous, flattened anteriorly, unduly enlarged or small.
·
Skin – Striaegravidarum
and lineanigra
·
Scar of previous
operations
·
Prominent veins, evidence
of skin infections
·
Umbilicus - Flat and
dimple
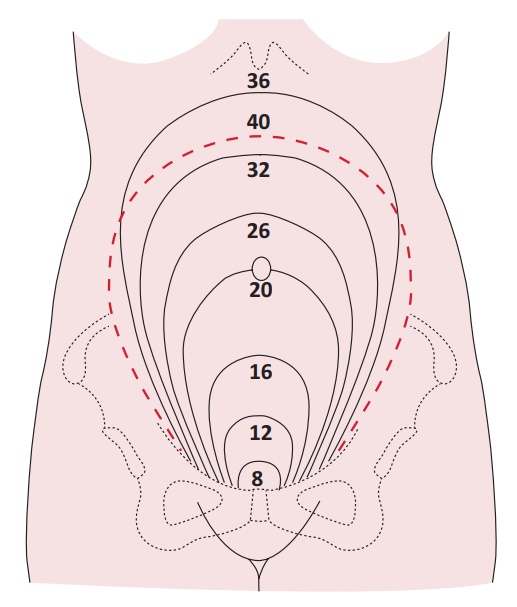
Uterus Size
12 Weeks-at the level of symphysis pubis
16 weeks- Half way between symphysis pubis
22 weeks- at the level of umbilicus
28 weeks- between umbilicus and Xiphoid process
32 weeks- below the xiphoid process
38 weeks- level of the xiphoid process
48 weeks- below the xiphoid process (if lightening occurs).
Palpation
·
Measure symphysis pubis
- fundal height
·
Between 18-34 weeks
measurements from pubis symphysis to the top of the uterus in cm correlates
well with the weeks of gestation
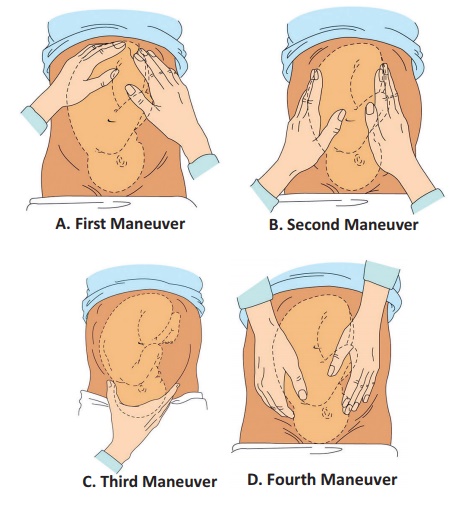
Abdominal –palpation
·
Measuring fundal height
(Leopold maneuver).
·
Fundal palpation(first
maneuver)
·
lateral palpation(second
maneuver)
·
Pelvic grip-I
·
Pelvic grip-II(Pawlik’s
grip)
Feel for presenting part
·
Determine lie
·
Determine position of
the presenting part
·
Engagement

Auscultation
Fetal heart rates can be identified by Doppler ultrasound by 12 –
24 weeks and by fetoscope at 18– 20 weeks.
Investigations
·
Urine test for
confirmation of pregnancy, albumin and sugar
·
Blood test for
1.
grouping
2.
Rh-typing
3.
Blood sugar
4.
Haemoglobin
5.
HIV Antigen.
6.
VDRL
7.
HbsAg.
2. Antenatal Advice
Nutrition
·
Weight gain - the
recommended weight gain in a normal pregnancy is 11.5 to 16 kg. Failure to
weight gain may lead to IUGR, Low birth weight babies and poor perinatal
outcome. Excessive weight gain may be due to fluid retention pre-eclampsia.
·
Calories & proteins
– The pregnant women require 300 kcal/day protein promotes growth of the fetus,
placenta, uterus, breast, red cells and production of milk. During pregnancy 1
g of protein is deposited half to the fetus and half to mothers.
·
Fats – Fats are
important sources of energy. Phospholipids lower the surface tension in the
lungs of the newborn.
·
Iron – Recommended iron
intake is 30 – 60 mg of elemental iron per day. During pregnancy iron stores
are depleted, supplementary iron is needed for both mother and fetus.
·
Calcium – Recommended
calcium intake is 1200 mg per day.
·
Vitamins – Folic acid is
required for the formation of heme. Deficiency of folic
acid may cause megaloblastic anaemia and neural tube defect in
fetus.
Life Style Modification
·
Exercise– It is not
necessary for a pregnant mother to limit her exercise but restriction may
require in Placenta previa, Cervical incompetence, Pregnancy induced
hypertension, Premature labour and multiple gestation.
·
Travel – No harmful
effects have been identified. A pregnant woman should move around every 2 hours
to prevent venous stasis and thrombus formation.
·
Bowel habit in pregnancy
due to progesterone induced GI smooth muscle relaxes lead to increased transit
time. Late in pregnancy compression on the bowel by the presenting part may cause
constipation. Women may avoid constipation by liberal fluid intake, exercise
and stool softner, bulking agents & mild laxatives.
·
Nausea & vomiting
are common in the first and second trimesters, usually in the morning. Small
frequent meals and avoidance of strong odours.
·
Sexual intercourse does
no harm but should be avoided if there is pregnancy complication such as
placenta praevia, rupture of membrane, preterm labour.
·
Smoking– women who smoke
often have smaller infants with increased perinatal morbidity. Mothers are
encouraged to quit smoking completely during pregnancy.
·
Alcohol should not be
consumed during pregnancy. The fetal abnormalities associated with drinking
(fetal alcoholic syndrome) include craniofacial defects, limb and CVS defects,
prenatal and postnatal growth restriction and mental retardation.
Caffeine has no increase in teratogenic or reproductive risk.
Related Topics