Chapter: Essentials of Psychiatry: Group Psychotherapy
Group Psychotherapy: Beginning a Group
Beginning
a Group
Group Organization
Forming a
psychotherapy group is a complex task and attention to organizational details
will anticipate some of the potential haz-ards and smooth the path.
Composition, size, fees, place, duration and time of meetings are elements that
require decisions in ad-vance of recruiting and preparing potential members.
The size
of dynamically-oriented groups ranges from six to 10 members. Groups at the
upper size range generally meet for lengthier periods to provide sufficient
“airtime” for each person. Smaller groups (four members or less) may be
threatened by fears of dissolution (Fulkerson et al., 1981). The duration of meetings is set for 75 to 120
minutes, the norm being 90 minutes. Most groups meet once weekly. Attention
must be paid to the group space. An optimal room will comfortably seat eight to
10 persons with unobstructed views of one another. Seats do not have to be
identical. Both the position and the type of seat members choose may assume
considerable emotional significance. Access to the room needs consideration. Is
there time for members to gather in the group room before the meeting, or is a
waiting room necessary? In private settings, meetings are occasionally held in
a waiting room and therapists must ensure that others do not intrude on that
space.
Careful
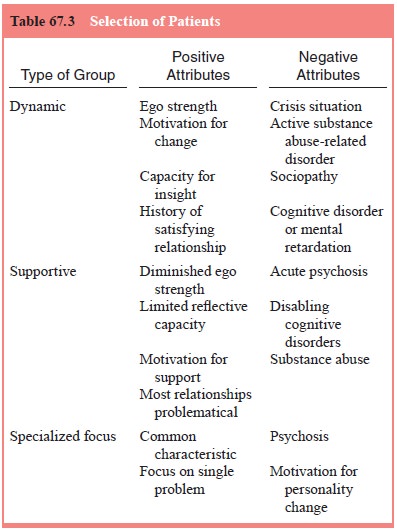
thought must be given to optimal group composi-tion (Table 67.3). Patients
chosen for groups that will explore in-trapsychic elements should have a
capacity for self-reflection and empathy with others. If possible, members with
different person-ality styles should be selected to provide a spectrum of
interac-tive patterns. Other long-term groups may be established with
supportive goals and include patients with significant ego deficits. (Groups
for the chronically mentally ill are discussed separately later.) Groups
designed with a specialized format (e.g., women survivors of sexual abuse, male
perpetrators, or individuals with eating disorders) generally are more focused
on a symptom or a specific behavior and in such cases balanced membership is of
lesser importance.
Recruiting, Selecting and Preparing Patients
Few
applicants requesting psychotherapy consider group treatment. Thus, gathering
six to 10 individuals together may not be a simple task. Patients are more
likely to agree to enter a group if the rationale is explained to them in some
detail. Thus, the therapist needs to be clear about the relationship between
group goals and patient goals (to be discussed below). The therapist also needs
to be familiar with the patient’s history, coping style, symptoms and
personality configurations. In obtaining a patient’s developmental history, the
therapist can specifically search for the person’s interaction in group
settings, such as school, church, recreation and family. Discussion of the
person’s typical reactions to group situations helps engage the patient in
examining his or her roles in interpersonal situations. The screening and
preparatory interviews have five major tasks (Rutan and Stone, 2001):
·
Establish a preliminary alliance between patient
and therapist.
·
Define the patients’ therapeutic goals.
·
Provide information about the nature of group
treatment.
·
Explore the patients’ anticipatory anxiety.
·
Discuss the group agreement and gain the patient’s
acceptance.
Careful
screening helps patients anticipate the tasks of en-tering a group. Such
preparation will decrease, but not eliminate premature termination which may
range from 20 to 50% of mem-bers in newly formed groups.
The Group Agreement
The
agreement represents the framework in which treatment will proceed. It promotes
a structure that defines boundaries between
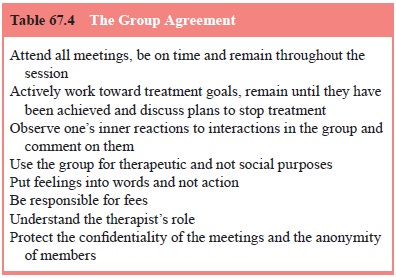
the group
and the environment, among the members and with the therapist. Although members
accept the agreement, they also break it. Such disruptions are valuable windows
into understand-ing a person’s inner world. The therapist must distinguish
be-tween acts that are disruptive to the group and those that carry more benign
communications (Nitsun, 1996).
Rutan and
Stone (2001) list the elements of the agreement as shown in Table 67.4.
The
initial element in the agreement addresses patients’ ability to attend all
sessions. Those who have responsibilities that interfere with attendance should
not be admitted into the group (e.g., executives whose conflicts make them
unavailable once every third or fourth week). Similarly, persons who have time
conflicts and would consistently come late or leave early should delay entry
until their schedule can be adapted to that of the group.
In
establishing goals, the patient and therapist enter into a conscious agreement
to work toward specified change. However, unconscious elements contributing to
a patient’s behaviors are likely to emerge in the therapeutic process that may
point to ad-ditional goals worthy of pursuit. Instructions regarding
termina-tion are an additional part of this agreement element. Patients generally
have little idea how to stop treatment, and leaders can indicate that
sufficient time to take leave of the group is an im-portant part of the
therapy. Plans to leave should be discussed and then a date for departure
established that allows sufficient time to say goodbye.
The
succeeding three elements in the agreement address patient behaviors within the
group. Patients slowly learn that one of the major benefits of therapy follows
from addressing feelings and reactions to one another and to the therapist.
Consistent at-tainment of this goal suggests that the group is functioning at a
mature level. Physical contact and verbal abuse are prohibited. Patients unable
to contain these behaviors may be asked to leave the session temporarily.
Although physical touching or hugging may seem soothing and reassuring to some
individuals, for oth-ers it is a threat to their personal boundaries. Those
behaviors are open to analysis.
Therapist’s Role
The group
leader assumes a major, but not the sole, responsibil-ity for the treatment.
The therapist’s special role is established in part by the agreement. Within
that framework, clinicians begin to shape the group to provide participants a
way of using their experience to learn about themselves. Assuming that
patients’
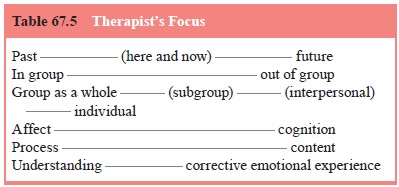
optimal
learning begins with a focus on transactions within the group,
psychodynamically-oriented therapists try to find ways of helping members
examine resistances and defenses against such engagement. In contrast,
clinicians using a more strictly interper-sonal (Yalom, 1995) or a
system-centered orientation (Agazarian, 1997) may actively instruct members to
address one another directly in the here and now of the meeting. The goals of
the different approaches are similar: to use the intragroup processes to
promote personal change. Therapists always benefit from ex-amining their own
contributions to the construction of the group dialogue. The therapist’s focus,
however, is not exclusively on in-group processes. Rutan and Stone (2001) list
six foci for the therapist’s attention (Table 67.5):
The major
but not exclusive focus promoting change is members learning from the here and
now of treatment. Groups develop a rhythm in which members might address
outside events as a warm-up to exploring in-group interactions, or they might
focus on current feelings and then expand on those experiences in respect to
their outside lives, now, in the past, or in the future. Integration of a
person’s experiences across an extended period enhances feelings of continuity
and stability of the self.
The
therapist monitors the ebb and flow of affects which reflect the group
developmental stage. Members’ capacity to tol-erate intense feelings is
enhanced as trust and cohesion increase. The dialectical tension between affect
and cognition is seen in members’ roles as they attempt to contain dysphoric
states and sustain emotional contacts with one another. Patients may find ways
of managing intense feelings through scapegoating or ex-ternalizing. These are
group-wide processes and should be ad-dressed as such. Some individuals require
cognitive understand-ing before risking immersion into feelings, whereas others
search for affective connections before integrating their experience
cognitively.
The
therapeutic process is fueled by members’ searching for new solutions to their
developmental arrests and conflicts. In general, members communicate feelings
about their in-group ex-perience through associations (not always conscious) to
events in their outside world. As such, the associations can be understood as
metaphoric communication that informs the treatment proc-ess. After a
successful interpretation or clarification, associations to external or
historical events may represent integration of those experiences into members’
psychic structure.
Considerable
individual change takes place via the group relationship without overt
cognitive integration. The sense of sharing, of being understood, of having
needs met, of being responded to in an empathic (corrective) manner may stabilize
a shaky psychic structure and, some patients, to their therapist’s surprise,
may successfully terminate treatment without having achieved understanding
(Stone, 1985). These are the powerful forces for change, labeled “corrective
emotional” experiences. Patients also strive for cognitive integration of their
thoughts andfeelings and, through experiencing and then understanding the
here-and-now, external and developmental incidents, they con-solidate their
learning. Patients are then more prepared to trans-fer their learning from
therapy to situations in their outside world (Ezriel, 1973).
Members’
level of self and ego development influence the course of the group as a
therapeutic agent. Persons suffering from archaic conflicts of trust or psychic
safety, as expressed in a vari-ety of personality disorders (the difficult
patient), may require an extended period of therapy exploring these issues.
Transferences to the group, leader, or peers emerge that reflect these
develop-mental levels.
Related Topics