Chapter: Medicine and surgery: Nervous system
Gliomas (astrocytomas and oligodendrogliomas) - Tumours of the nervous system
Gliomas (astrocytomas and oligodendrogliomas)
Definition
Tumours with histological appearances of glial cells – the scaffolding cells of the CNS.
· Astrocytomas have predominantly astrocytic cells. They are categorised according to their histological appearance into low grade astrocytoma (WHO grade 2), anaplastic astrocytoma (WHO grade 3) and glioblastoma multiforme (WHO grade 4).
· Oligodendromas arise from the oligodendrocytes (CNS myelinating cells) and usually behave as low-grade tumours.
· Mixed glial tumours with astrocytic and oligodendroglial components occur and are termed oligoastrocytoma.
Aetiology
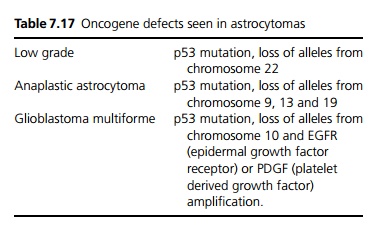
Astrocytomas occur anywhere in the brain. Oligoden-drogliomas tend to arise in the cerebral hemispheres. Glioblastomas are the most aggressive pleomorphic type of glial cell tumour. Oncogene defects seen in astrocy-tomas are shown in Table 7.17.
Pathophysiology
Tumours do not metastasise but can spread locally by infiltration. There is also a risk that a low grade tumour may become more aggressive.
Clinical features
Most patients present with focal neurological signs and headache or signs of raised intracranial pressure. Convulsions may occur. The rapidity of onset of symptoms is often an indication of the aggressiveness of the tumour.
Investigations
Neuroimaging with CT or MRI – the latter is more sensitive and provides greater anatomical detail. Astrocytomas are usually highly vascular and enhance with contrast in over two-thirds of cases (less often in lowgrade astrocytoma). Surrounding oedema is commonly seen, but due to the diffuse infiltration, the limits of oedema often demarcate the limits of the tumour spread. For this reason, prior use of corticosteroids can reduce the appearance of the size of the tumour. Oligodendromas commonly calcify. CT is less useful then MRI.
Biopsy – stereotactic biopsy (linking information for CT and MRI to guide surgery via surface landmarks or a frame to achieve accuracy to within 1 mm) is used which increases sensitivity, and reduces morbidity and mortality.
Macroscopy/microscopy
Astrocytomas are illdefined pale areas which are not clearly demarcated from the adjacent brain. The cells look like astrocytes and there are different histological patterns.
Oligodendrogliomas are macroscopically similar to astrocytomas, arising as greyish white lesions that are not clearly differentiated from the surrounding tissue. The cells have round nuclei and pale vacuolated cytoplasm (fried egg appearance).
Glioblastoma muliforme tumours may be necrotic, haemorrhagic masses due to rapid growth. They are composed of pleomorphic cells.
Management
It is still unclear whether early complete surgical removal of low-grade tumours that cause little or transient neurology improves the prognosis; although surgery is helpful for reducing the need for treatment of seizures, it has the disadvantage of often causing major neurological deficit.
For astrocytomas, complete surgical removal is difficult due to the diffuse nature and difficulty in determining the limits of the tumour. For high-grade astrocytomas, in many cases the tumour is unresectable. Even if the tumour is resectable, the high risk of recurrence, together with the major morbidity of surgery may mean debulking surgery only and treatment with radiotherapy and/or chemotherapy.
Hydrocephalus can be treated with a shunt. Seizures are treated with antiepileptic drugs.
Prognosis
Lowgrade tumours grow slowly over many years while glioblastoma multiforme causes death within months.
Related Topics