Chapter: Medical Surgical Nursing: Genetics Perspectives in Nursing
Genetic Counseling and Evaluation Services - Applications of Genetics in Nursing Practice
GENETIC
COUNSELING AND EVALUATION SERVICES
As the contribution of genetics to the health–illness continuum is
recognized, the process of genetic counseling is expected to be-come a
responsibility of all health care professionals in clinical practice. Nurses
are obvious and natural providers of genetics services because they are aware
of a patient’s personal and family history. They assess patients’ health and
make referrals for spe-cialized diagnosis and treatment. They offer
anticipatory guidance by explaining the purpose and goals of a referral. They
collabo-rate with primary care providers and specialists in giving sup-portive
and follow-up counseling. They coordinate follow-up and case management.
Genetics Services
Genetics services provide genetics information, education, and support to patients and families with genetics-related health concerns.
Genetics professionals, including medical geneticists, genetics counselors, and advanced practice nurses in genetics, provide
specific genetics services to patients and families who are referred by their
primary health care providers. A team approach is often used by genetics
specialists to obtain and interpret com-plex family history information,
evaluate and diagnose genetic conditions, interpret and discuss complicated
genetic test results, support patients throughout the evaluation process, and
offer re-sources for additional professional and family support. Patients
participate as team members and decision-makers throughout the process.
Genetics services encompass an evaluation and commu-nication process by which
individuals and their families come to learn and understand relevant aspects of
genetics, to make in-formed health decisions, and to receive support as they
integrate personal and family genetics information into daily living (Lea,
Jenkins & Francomano, 1998).
Genetic counseling may take place over an extended period and may entail
more than one counseling session, which may in-clude other family members. This
allows patients and families to learn and understand genetics information, to
receive support and guidance in decision-making, and to obtain comprehensive
and coordinated care if they have specific genetic conditions or concerns. The
components of genetic counseling are outlined in Chart 9-6. Genetic counseling
may be offered at any point during the lifespan, although genetic counseling
issues are often relevant to the life stage in which counseling is sought. Some
ex-amples are presented in Chart 9-7 (Lea, Jenkins & Francomano, 1998).
Nursing Role in Genetic Counseling
Patients seek genetic counseling for a variety of reasons and at
dif-ferent stages of life. Some are seeking preconception or prenatal
information; others are referred following the birth of a child with a birth
defect or suspected genetic condition; still others are seek-ing information
for themselves or their families because of the presence or family history of a
genetic condition. Regardless of the timing or setting, genetic counseling is
offered to all patients who have questions about genetics and their health. In
collabo-ration with the health care team, the nurse considers referring for
genetic counseling any patient in whose family a heritable condition exists and who asks
questions such as, “What are my chances for having this condition? Is there a
genetic test that will tell me? Is there a genetic treatment or cure? What are
my options?” (Lea, Jenkins & Francomano, 1998).
Nurses refer clients,
collaborate with genetics specialists, and participate in genetic counseling
when they carry out the follow-ing activities:
· Provide appropriate
genetic information before, during, and in follow-up to genetic counseling
· Help gather relevant
family and medical history information
· Offer support to
patients and families throughout the ge-netic counseling process
· Coordinate
genetics-related health care with relevant com-munity and national support
resources
These activities,
carried out in collaboration with patients and families, help ensure that they
receive the most benefit from genetic counseling (Lea, Jenkins &
Francomano, 1998; Lea, Williams, Jenkins, et al., 2000).
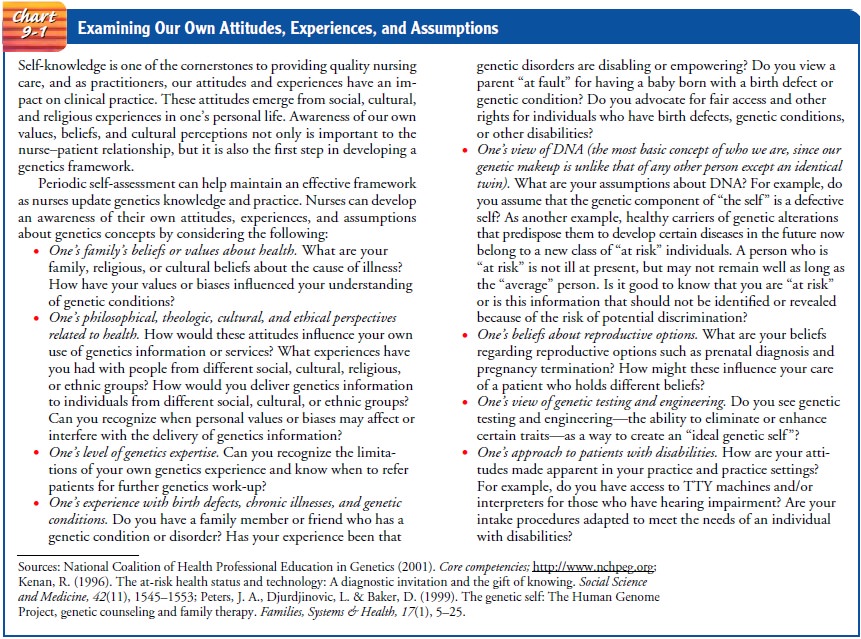
RESPECTING PATIENTS’ RIGHTS
Respecting the patient’s right to self-determination—that is,
sup-porting decisions that reflect the patient’s personal beliefs, values, and
interests—is a central principle of how nurses provide genet-ics information
and counseling. Genetics specialists and nurses participating in genetic
counseling make every attempt to respect the patient’s ability to make
autonomous decisions. A first step in providing such nondirective counseling is
recognizing one’s own values (see Chart 9-1) and how communication of genetics
in-formation may be influenced by those values.
Confidentiality of genetics information and respect for privacy are other essential principles underlying genetic counseling. The patient has the right to have testing without having the results di-vulged to anyone, including insurers or physicians. Some patients pay for testing themselves so that insurers will not learn of the test; others use a different name for testing to protect their pri-vacy. The Health Insurance Portability and Accountability Act (HIPAA) of 1996 prohibits the use of genetics information to es-tablish insurance eligibility. However, it does not prohibit group plans from increasing premiums, excluding coverage for a specific condition, or imposing a lifetime cap on benefits. The National Human Genome Research Institute, Policy and Public Affairs and Legislative Activities Branch has a summary of each state’s legislation on employment and insurance discrimination.
All genetics specialists, including nurses who participate in the
genetic counseling process and those with access to individuals’ genetic
information, must honor the patient’s desire for confi-dentiality. Genetics
information should be kept from family members, insurance companies, employers,
and schools if the pa-tient desires, even if keeping the information
confidential is dif-ficult. The nurse may want to disclose genetics information
to family members who could experience significant harm if they do not know
such information. However, the patient may have other views and may wish to
keep this information from the family, re-sulting in an ethical dilemma for
both patient and nurse. The nurse must honor the patient’s wishes while
explaining to the pa-tient the potential benefit this information may have to
other family members (ISONG, 2002).
PROVIDING PRECOUNSELING INFORMATION
Preparing the patient and family, promoting informed decision-making,
and obtaining informed consent are essential in genetic counseling. The nurse
assesses the patient’s capacity and ability to give voluntary consent. This
includes assessment of factors that may interfere with informed consent such as
hearing and lan-guage deficits, impaired intelligence, and the effects of
medication. The nurse makes sure that the individual’s decision to un-dergo
testing is not affected by coercion, persuasion, or manipu-lation. Because
information may need to be repeated over time, the nurse offers follow-up
discussion as needed (Bove et al., 1997).
The genetics service to which the nurse refers a patient or fam-ily for
genetic counseling will ask the nurse to provide back-ground information for
evaluation. Genetics specialists need to know the reason for referral, the
patient’s or family’s reason for seeking genetic counseling, and potential
genetics-related health concerns. The nurse may refer a family with a new
diagnosis of hereditary breast or ovarian cancer, for example, to obtain more
information or counseling or to discuss the likelihood of devel-oping the
disease and the implications for other family members. The family may have
concerns about confidentiality and privacy. Using the nursing assessment, the
genetics specialists tailor the genetic counseling to respond to these
concerns.
With the patient’s permission, the nurse may also provide to the
genetics specialists the relevant test results and medical eval-uations. The
nurse needs to obtain permission from the patient and, if applicable, from
other family members to retrieve, review, and transfer medical records that
document the genetic condition of concern. In some situations, evaluation of
more than one fam-ily member may be necessary to establish a diagnosis of a
genetic disorder. The nurse can prepare the family for this assessment by
explaining that the medical information and evaluation are nec-essary to ensure
that appropriate information and counseling (in-cluding risk interpretation)
are provided.
The nurse will be asked to provide information about the emotional and
social status of the patient and family. Genetics specialists will want to know
the coping skills of a family that has recently learned of the diagnosis of a
genetic disorder. They will want to be aware of the types of genetics
information being sought. The nurse helps to identify cultural and other issues
that may influence how information is provided and by whom. For patients with
hearing loss, for example, an interpreter’s services may have to be arranged.
The genetics professional, after deter-mining these issues with the nurse,
prepares for the genetic coun-seling and evaluation with these relevant issues
in mind (Lea, Jenkins & Francomano, 1998).
PREPARING THE PATIENT FOR GENETIC EVALUATION
Before the genetic counseling appointment, the nurse discusses with the
patient and family the type and nature of family history information that will
be collected during the consultation. Family history collection and analysis
are comprehensive and focus on information that may be relevant to the specific
genetic concern in question. Although targeted to each genetic counseling
situation, such analysis always includes assessment for any other potentially
inherited conditions for which testing and preventive and treat-ment measures
may be offered.
A physical examination
performed by the medical geneticist may be needed to identify specific clinical
features that are diag-nostic of a genetic condition. The examination also
helps to iden-tify whether additional laboratory tests are needed to clarify
the diagnosis of a genetic disorder. The detailed physical examination
generally involves assessment of all body systems, with a focus on specific
physical characteristics considered for diagnosis. The nurse describes the
diagnostic evaluations that are part of a ge-netics consultation and explains
their purposes (Lashley, 1998; Lea, Jenkins & Francomano, 1998).
COMMUNICATING GENETICS INFORMATION TO THE PATIENT
After the family history and physical examination are completed, the
genetics team reviews the information gathered before begin-ning genetic
counseling with the patient and family. The genet-ics specialists meet with the
patient and family to discuss their findings. When information from family and
medical histories and examination confirms the presence of a genetic condition
in a family, the genetics specialist discusses with the patient the nat-ural
history of the condition, the pattern of inheritance, and the implications of
the genetic condition for reproductive and gen-eral health. When appropriate,
the genetic specialists discuss and describe relevant testing and management
options. The nurse as-sesses the patient’s understanding of the genetic
consultation and clarifies information given by the specialists.
PROVIDING SUPPORT
The genetics team provides support throughout the counseling session and
makes every effort to elicit individual and family con-cerns. The genetics
specialist uses principles of active listening to interpret patient concerns
and emotions, seek and provide feed-back, and demonstrate understanding of
those concerns. When needed, the genetics specialist suggests referral for
additional social and emotional support. The genetics specialist discusses
pertinent patient and family concerns and needs with the nurse and primary
health care team so that they can provide additional support and guidance (Lea,
Jenkins & Francomano, 1998). The nurse assesses the patient’s understanding
of the information given during the counseling session, clarifies information,
an-swers questions, assesses the patient’s reactions, and identifies supports.
Providing Follow-Up After Genetic Evaluation
In follow-up to genetic evaluation and counseling, the genetics
specialists prepare a written summary of the evaluation and coun-seling session
and, with the patient’s permission, send this sum-mary to the primary health
care provider as well as all other providers and participants in the patient’s
care, as identified by the family. The consultation summary outlines the
results of fam-ily history and physical and laboratory assessments, provides a
discussion of the specific diagnosis (when made), reviews the in-heritance and
associated risk of recurrence for the patient and family, presents reproductive
and general health options, and makes recommendations for further testing and
management. The summary is also sent to the patient and a copy is retained in
the patient’s medical records. The nurse has an important role in reviewing the
summary with the patient and family and identify-ing information, education,
and counseling for which follow-up genetic counseling may be useful (Lea,
Jenkins & Francomano, 1998; Lea & Williams, 2002; Lea & Smith,
2002).
Follow-up genetic counseling is always offered to patients and families,
as some may need more time to understand and discuss the specifics of a genetic
test or diagnosis or wish to review re-productive options again later when
pregnancy is being consid-ered. Follow-up genetic counseling is also offered to
clients when further evaluation and counseling of extended family members is
recommended (Lea, Jenkins & Francomano, 1998).
As part of follow-up, nurses can educate patients about where to find
information about genetics issues. Some resources that provide the most
up-to-date and reliable genetics information are available on the Internet.
Related Topics