Chapter: Medical Physiology: Adrenocortical Hormones
Functions of the Mineralocorticoids- Aldosterone
Functions of the Mineralocorticoids- Aldosterone
Mineralocorticoid Deficiency Causes Severe Renal Sodium Chloride Wasting and Hyperkalemia. Total loss of adreno-cortical secretion usually causes death within 3 days to 2 weeks unless the person receives extensive salt therapy or injection of mineralocorticoids.
Without mineralocorticoids, potassium ion concen-tration of the extracellular fluid rises markedly, sodium and chloride are rapidly lost from the body, and the total extracellular fluid volume and blood volume become greatly reduced. The person soon develops diminished cardiac output, which progresses to a shocklike state, followed by death. This entire sequence can be prevented by the administration of aldosterone or some other mineralocorticoid. There-fore, the mineralocorticoids are said to be the acute “lifesaving” portion of the adrenocortical hormones. The glucocorticoids are equally necessary, however, allowing the person to resist the destructive effects of life’s intermittent physical and mental “stresses,”.
Aldosterone Is the Major Mineralocorticoid Secreted by the Adrenals. Aldosterone exerts nearly 90 per cent of themineralocorticoid activity of the adrenocortical secre-tions, but cortisol, the major glucocorticoid secreted by the adrenal cortex, also provides a significant amount of mineralocorticoid activity. Aldosterone’s mineralo-corticoid activity is about 3000 times greater than that of cortisol, but the plasma concentration of cortisol is nearly 2000 times that of aldosterone.
Renal and Circulatory Effects of Aldosterone
Aldosterone Increases Renal Tubular Reabsorption of Sodium and Secretion of Potassium. It will be recalled that aldosterone increases absorption of sodium and simultaneously increases secretion of potassium by the renal tubular epithelial cells especially in the principal cells of the collecting tubules and, to a lesser extent, in the distal tubules and col-lecting ducts. Therefore, aldosterone causes sodium to be conserved in the extracellular fluid while increasing potassium excretion in the urine.
A high concentration of aldosterone in the plasma can transiently decrease the sodium loss into the urine to as little as a few milliequivalents a day. At the same time, potassium loss into the urine increases several-fold. Therefore, the net effect of excess aldosterone in the plasma is to increase the total quantity of sodium in the extracellular fluid while decreasing the potassium.
Conversely, total lack of aldosterone secretion can cause transient loss of 10 to 20 grams of sodium in the urine a day, an amount equal to one tenth to one fifth of all the sodium in the body. At the same time, potas-sium is conserved tenaciously in the extracellular fluid.
Excess Aldosterone Increases Extracellular Fluid Volume and Arterial Pressure but Has Only a Small Effect on Plasma Sodium Concentration. Although aldosterone has a potenteffect in decreasing the rate of sodium ion excretion by the kidneys, the concentration of sodium in the extracellular fluid often rises only a few milliequiva-lents. The reason for this is that when sodium is reab-sorbed by the tubules, there is simultaneous osmotic absorption of almost equivalent amounts of water. Also, small increases in extracellular fluid sodium concentration stimulate thirst and increased water intake, if water is available. Therefore, the extracellu-lar fluid volume increases almost as much as the retained sodium, but without much change in sodium concentration.
Even though aldosterone is one of the body’s most powerful sodium-retaining hormones, only transient sodium retention occurs when excess amounts are secreted. An aldosterone-mediated increase in extra-cellular fluid volume lasting more than 1 to 2 days also leads to an increase in arterial pressure. The rise in arterial pressure then increases kidney excretion of both salt and water, called pressure natriuresis and pressure diuresis, respectively. Thus, after the extracellular fluid volume increases 5 to 15 per cent above normal, arterial pres-sure also increases 15 to 25 mm Hg, and this elevated blood pressure returns the renal output of salt and water to normal despite the excess aldosterone (Figure77–3).
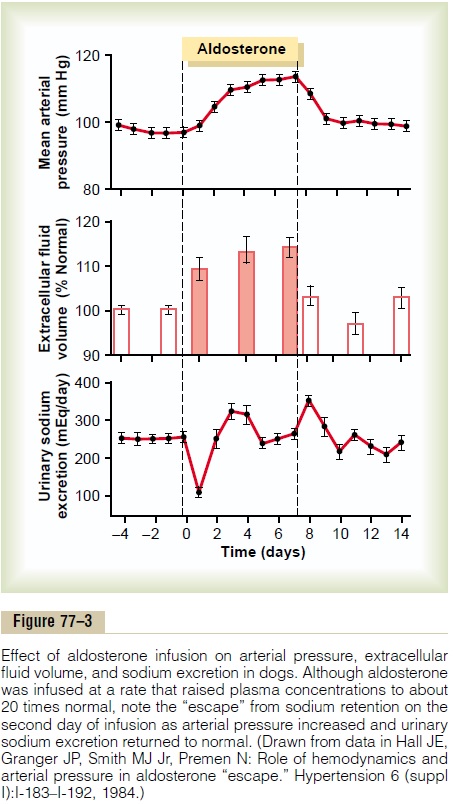
This return to normal of salt and water excretion by the kidneys as a result of pressure natriuresis and diuresis is called aldosterone escape. Thereafter, the rate of gain of salt and water by the body is zero, and balance is maintained between salt and water intake and output by the kidneys despite continued excess aldosterone. In the meantime, however, the person has developed hypertension, which lasts as long as the person remains exposed to high levels of aldosterone.
Conversely, when aldosterone secretion becomes zero, large amounts of salt are lost in the urine, not only diminishing the amount of sodium chloride in the extracellular fluid but also decreasing the extracellular fluid volume. The result is severe extracellular fluid dehydration and low blood volume, leading to circula-tory shock. Without therapy, this usually causes deathwithin a few days after the adrenal glands suddenly stop secreting aldosterone.
Excess Aldosterone Causes Hypokalemia and Muscle Weak-ness; Too Little Aldosterone Causes Hyperkalemia and Cardiac Toxicity. Excess aldosterone not only causes loss ofpotassium ions from the extracellular fluid into the urine but also stimulates transport of potassium from the extracellular fluid into most cells of the body. Therefore, excessive secretion of aldosterone, as occurs with some types of adrenal tumors, may cause a serious decrease in the plasma potassium concentration, sometimes from the normal value of 4.5 mEq/L to as low as 2 mEq/L. This condition is called hypokalemia. When the potassium ion concen-tration falls below about one-half normal, severe muscle weakness often develops. This is caused by alteration of the electrical excitability of the nerve and muscle fiber membranes, which pre-vents transmission of normal action potentials.
Conversely, when aldosterone is deficient, the extra-cellular fluid potassium ion concentration can rise far above normal.When it rises to 60 to 100 per cent above normal, serious cardiac toxicity, including weakness of heart contraction and development of arrhythmia, becomes evident; progressively higher concentrations of potassium lead inevitably to heart failure.
Excess Aldosterone Increases Tubular Hydrogen Ion Secretion, and Causes Mild Alkalosis. Aldosterone not only causespotassium to be secreted into the tubules in exchange for sodium reabsorption in the principal cells of the renal collecting tubules but also causes secretion of hydrogen ions in exchange for sodium in the interca-lated cells of the cortical collecting tubules. Thisdecreases the hydrogen ion concentration in the extra-cellular fluid, causing a mild degree of alkalosis.
Aldosterone Stimulates Sodium and Potassium Transport in Sweat Glands, Salivary Glands, and Intestinal Epithelial Cells
Aldosterone has almost the same effects on sweat glands and salivary glands as it has on the renal tubules. Both these glands form a primary secretion that contains large quantities of sodium chloride, but much of the sodium chloride, on passing through the excretory ducts, is reabsorbed, whereas potassium and bicarbonate ions are secreted. Aldosterone greatly increases the reabsorption of sodium chloride and the secretion of potassium by the ducts. The effect on the sweat glands is important to conserve body salt in hot environments, and the effect on the salivary glands is necessary to conserve salt when excessive quantities of saliva are lost.
Aldosterone also greatly enhances sodium absorp-tion by the intestines, especially in the colon, which prevents loss of sodium in the stools. Conversely, in the absence of aldosterone, sodium absorption can be poor, leading to failure to absorb chloride and other anions and water as well. The unabsorbed sodium chloride and water then lead to diarrhea, with further loss of salt from the body.
Cellular Mechanism of Aldosterone Action
Although for many years we have known the overall effects of mineralocorticoids on the body, the basic action of aldosterone on the tubular cells to increase transport of sodium is still not fully understood. However, the cellular sequence of events that leads to increased sodium reabsorption seems to be the following.
First, because of its lipid solubility in the cellular membranes, aldosterone diffuses readily to the interior of the tubular epithelial cells.
Second, in the cytoplasm of the tubular cells, aldos-terone combines with a highly specific cytoplasmic receptor protein, a protein that has a stereomolecularconfiguration that allows only aldosterone or very similar compounds to combine with it.
Third, the aldosterone-receptor complex or a product of this complex diffuses into the nucleus, where it may undergo further alterations, finally induc-ing one or more specific portions of the DNA to form one or more types of messenger RNA related to the process of sodium and potassium transport.
Fourth, the messenger RNA diffuses back into the cytoplasm, where, operating in conjunction with the ribosomes, it causes protein formation. The proteins formed are a mixture of (1) one or more enzymes and (2) membrane transport proteins that, all acting together, are required for sodium, potassium, and hydrogen transport through the cell membrane. One of the enzymes especially increased is sodium-potassium adenosine triphosphatase, which serves asthe principal part of the pump for sodium and potas-sium exchange at the basolateral membranes of the renal tubular cells. Additional proteins, perhaps equally important, are epithelial sodium channel pro-teins inserted into the luminal membrane of the same tubular cells that allows rapid diffusion of sodium ions from the tubular lumen into the cell; then the sodium is pumped the rest of the way by the sodium-potassium pump located in the basolateral membranes of the cell.
Thus, aldosterone does not have an immediate effect on sodium transport; rather, this effect must await the sequence of events that leads to the formation of the specific intracellular substances required for sodium transport. About 30 minutes is required before new RNA appears in the cells, and about 45 minutes is required before the rate of sodium transport begins to increase; the effect reaches maximum only after several hours.
Possible Nongenomic Actions of Aldosterone and Other Steroid Hormones
Recent studies suggest that many steroids, including aldosterone, elicit not only slowly developing genomic effects that have a latency of 60 to 90 minutes and require gene transcription and synthesis of new pro-teins, but also rapid nongenomic effects that take place in a few seconds or minutes.
These nongenomic actions are believed to be medi-ated by binding of steroids to cell membrane receptors that are coupled to second messenger systems, similar to those used for peptide hormone signal transduction. For example, aldosterone has been shown to increase formation of cAMP in vascular smooth muscle cells and in epithelial cells of the renal collecting tubules in less than two minutes, a time period that is far too short for gene transcription and synthesis of new pro-teins. In other cell types, aldosterone has been shown to rapidly stimulate the phosphatidylinositol second messenger system. However, the precise structure of receptors responsible for the rapid effects of aldos-terone has not been determined, nor is the physiolog-ical significance of these nongenomic actions of steroids well understood.
Regulation of Aldosterone Secretion
The regulation of aldosterone secretion is so deeply intertwined with the regulation of extracellular fluid electrolyte concentrations, extracellular fluid volume, blood volume, arterial pressure, and many special aspects of renal function that it is difficult to discuss the regulation of aldosterone secretion independently of all these other factors. However, it is important to list here some of the more important points of aldosterone secretion control.
The regulation of aldosterone secretion by the zona glomerulosa cells is almost entirely independent of the regulation of cortisol and androgens by the zona fas-ciculata and zona reticularis.
Four factors are known to play essential roles in the regulation of aldosterone. In the probable order of their importance, they are as follows:
1. Increased potassium ion concentration in the extracellular fluid greatly increases aldosterone secretion.
2. Increased activity of the renin-angiotensin system (increased levels of angiotensin II) also greatly increases aldosterone secretion.
3. Increased sodium ion concentration in the extracellular fluid very slightly decreases aldosterone secretion.
4. ACTH from the anterior pituitary gland is necessary for aldosterone secretion but has little effect in controlling the rate of secretion.
Of these factors, potassium ion concentration and the renin-angiotensin system are by far the most potent in regulating aldosterone secretion. A small percentage increase in potassium concentration can cause a severalfold increase in aldosterone secretion. Likewise, activation of the renin-angiotensin system, usually in response to diminished blood flow to the kidneys or to sodium loss, can cause a severalfold increase in aldosterone secretion. In turn, the aldos-terone acts on the kidneys (1) to help them excrete the excess potassium ions and (2) to increase the blood volume and arterial pressure, thus returning the renin-angiotensin system toward its normal level of activity.
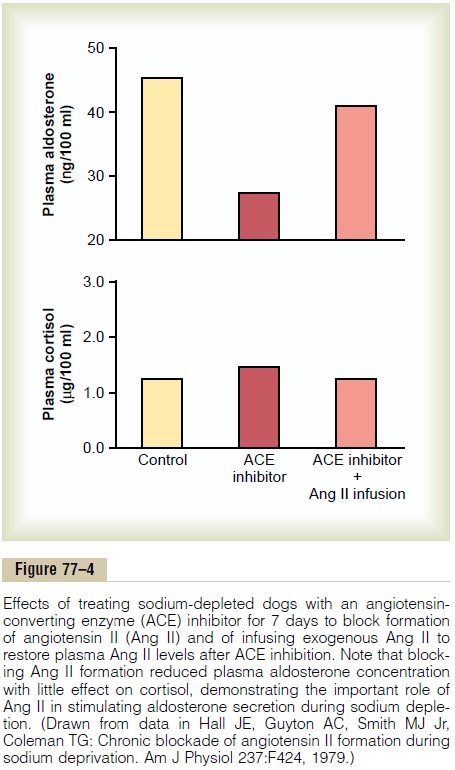
Figure 77–4 shows the effects on plasma aldosterone concentration caused by blocking the formation of angiotensin II with an angiotensin-converting enzyme inhibitor after several weeks of a low-sodium diet that increases plasma aldosterone concentration several-fold. Note that blocking angiotensin II formation markedly decreases plasma aldosterone concentration without significantly changing cortisol concentration; this indicates the important role of angiotensin II in stimulating aldosterone secretion when sodium intake and extracellular fluid volume are reduced.
By contrast, the effects of sodium ion concentration per se and of ACTH in controlling aldosterone secre-tion are usually minor. Nevertheless, a 10 to 20 per cent decrease in extracellular fluid sodium ion concentra-tion, which occurs on rare occasions, can perhaps double aldosterone secretion. In the case of ACTH, if there is even a small amount of ACTH secreted by the anterior pituitary gland, it is usually enough to permit the adrenal glands to secrete whatever amount of aldosterone is required, but total absence of ACTH can significantly reduce aldosterone secretion.
Related Topics