Chapter: Medical Surgical Nursing: Assessment of Digestive and Gastrointestinal Function
Function of the Digestive System
FUNCTION
OF THE DIGESTIVE SYSTEM
All
cells of the body require nutrients. These nutrients are derived from the
intake of food that contains proteins, fats, carbohydrates, vitamins and
minerals, and cellulose fibers and other vegetable matter of no nutritional
value. The primary digestive functions of the GI tract are the following:
•
To break down food particles into the molecular
form for digestion
•
To absorb into the bloodstream the small molecules
pro-duced by digestion
•
To eliminate undigested and unabsorbed foodstuffs
and other waste products from the body
After
food is ingested, it is propelled through the GI tract, coming into contact
with a wide variety of secretions that aid in its digestion, absorption, or elimination from the GI tract.
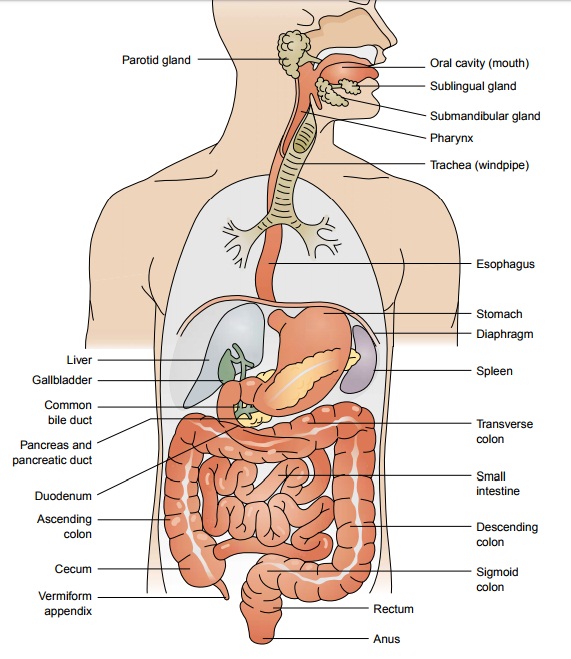
Chewing and Swallowing
The
process of digestion begins with the act of chewing, in which food is broken down
into small particles that can be swallowed and mixed with digestive enzymes.
Eating—or even the sight, smell, or taste of food—can cause reflex salivation.
Saliva is se-creted from three pairs of glands: the parotid, the submaxillary,
and the sublingual glands. Approximately 1.5 L of saliva is secreted daily.
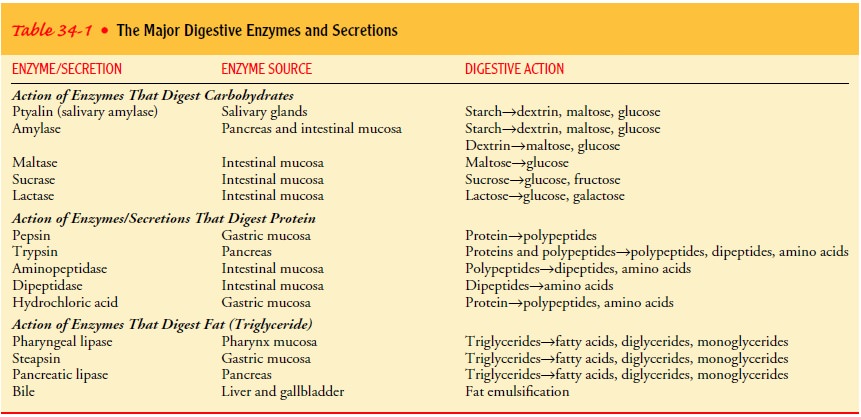
Saliva is the first secretion that comes in contact with food. Saliva contains
the enzyme ptyalin, or salivary amylase, which begins the digestion of starches
(Table 34-1). Saliva also contains mucus and water, which help to lubricate the
food as it is chewed, thereby facilitating swallowing.
Swallowing begins as a voluntary act that is regulated by a swal-lowing center in the medulla oblongata of the central nervous sys-tem. As food is swallowed, the epiglottis moves to cover the tracheal opening and prevent aspiration of food into the lungs. Swallowing, which propels the bolus of food into the upper esoph-agus, thus ends as a reflex action. The smooth muscle in the wall of the esophagus contracts in a rhythmic sequence from the upper esophagus toward the stomach to propel the bolus of food along the tract. During this process of esophageal peristalsis, the lower esophageal sphincter relaxes and permits the bolus of food to enter the stomach. Subsequently, the lower esophageal sphincter closes tightly to prevent reflux of stomach contents into the esophagus.
Gastric Function
The
stomach stores and mixes the food with secretions. It secretes a highly acidic
fluid in response to the presence or anticipated in-gestion of food. This fluid, which may have a pH as low as 1,
de-rives its acidity from the hydrochloric
acid (HCl) secreted by theglands of the stomach. The function of this
gastric secretion is two-fold: to break down food into more absorbable
components Aorta and to aid in the destruction of most ingested bacteria. The
stomach can produce about 2.4 L per day of these gastric secretions.Gastric
secretions also contain the enzyme pepsin, which is important for initiating
protein digestion. Intrinsic factor is also secreted by the gastric mucosa.
This compound combines with dietary vitamin B12 so that the vitamin can be
absorbed in the ileum. In the absence of intrinsic factor, vitamin B12 cannot
be absorbed and pernicious anemia results. Peristaltic contractions in the
stomach propel its contents toward the pylorus. Because large food particles
cannot pass through the pyloric sphincter, they are churned back into the body
of the stomach. In this way, food in the stomach is agitated mechanically and
broken down into smaller particles. Food remains in the stomach for a variable
length of time, from a half-hour to several hours, depending on the size of
food particles, the composition of the meal, and other factors. Peristalsis in
the stomach and contractions of the pyloric sphincter allow the partially
digested food to enter the small intestine at a rate that permits efficient
absorption of nutrients. This food mixed with gastric secretions is
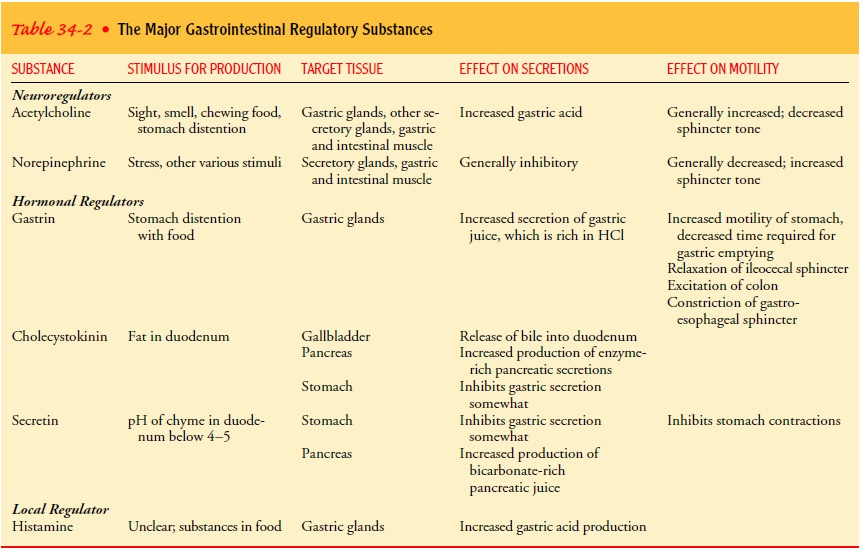
calledchyme. Hormones, neuroregulators, and local regulators found in the
gastric secretions control the rate of gastric secretions and influence gastric
motility (Table 34-2).
Small Intestine Function
The digestive process continues in the duodenum. Secretions in the duodenum come from the accessory digestive organs—the pancreas, liver, and gallbladder—and the glands in the wall of the intestine itself. These secretions contain digestive enzymes and bile. Pancreatic secretions have an alkaline pH because of high concentrations of bicarbonate. This neutralizes the acid entering the duodenum from the stomach. The pancreas also secretes di-gestive enzymes, including trypsin, which aids in digesting pro-tein; amylase, which aids in digesting starch; and lipase, which aids in digesting fats. Bile (secreted by the liver and stored in the gallbladder) aids in emulsifying ingested fats, making them easier to digest and absorb.
The
intestinal glands secrete mucus, hormones, electrolytes, and enzymes. The mucus
coats the cells and protects the mucosa from injury by HCl. Hormones,
neuroregulators, and local regulators found in these intestinal secretions
control the rate of intestinal se-cretions and also influence GI motility.
Intestinal secretions total approximately 1 L/day of pancreatic juice, 0.5
L/day of bile, and 3 L/day of secretions from the glands of the small
intestine. Ta-bles 34-1 and 34-2 summarize the actions of digestive enzymes and
GI regulatory substances.
Two
types of contractions occur regularly in the small intestine: segmentation
contractions and intestinal peristalsis. Segmentationcontractions
produce mixing waves that move the intestinal con-tents back and forth in a
churning motion. Intestinal peristalsis
pro-pels the contents of the small intestine toward the colon. Both movements
are stimulated by the presence of chyme.
Food,
initially ingested in the form of fats, proteins, and carbo-hydrates, is broken
down into absorbable particles (constituent nu-trients) by the process of
digestion. Carbohydrates are broken down into disaccharides (eg, sucrose,
maltose, galactose) and mono-saccharides (eg, glucose, fructose). Glucose is
the major carbohy-drate that the tissue cells use as fuel. Proteins are broken
down into amino acids and peptides. Ingested fats are emulsified into
mono-glycerides and fatty acids. These smaller molecules are then ready to be
absorbed. Chyme stays in the small intestine for 3 to 6 hours, allowing for
continued breakdown and absorption of nutrients.
Small,
finger-like projections called villi are present through-out the entire
intestine and function to produce digestive enzymes as well as to absorb
nutrients. Absorption is the primary function of the small intestine. Vitamins
and minerals are not di-gested but rather absorbed essentially unchanged.
Absorption be-gins in the jejunum and is accomplished by both active transport
and diffusion across the intestinal wall into the circulation. Ab-sorption of
different nutrients takes place at different locations in the small intestine.
Iron and calcium absorption takes place in the duodenum. Fats, proteins,
carbohydrates, sodium, and chloride are absorbed in the jejunum. Vitamin B12 and bile salts are
ab-sorbed in the ileum. Magnesium, phosphate, and potassium are absorbed
throughout the small intestine (Society of Gastroentero-logic Nursing and
Associates, 1998).
Colonic Function
Within
4 hours after eating, residual waste material passes into the terminal ileum
and passes slowly into the proximal portion of the colon through the ileocecal
valve. This valve, which is nor-mally closed, helps prevent colonic contents
from refluxing into the small intestine. With each peristaltic wave of the
small intes-tine, the valve opens briefly and permits some of the contents to
pass into the colon.
Bacteria
make up a major component of the contents of the large intestine. They assist
in completing the breakdown of waste material, especially of undigested or
unabsorbed proteins and bile salts. Two types of colonic secretions are added
to the resid-ual material: an electrolyte solution and mucus. The electrolyte
so-lution is chiefly a bicarbonate solution that acts to neutralize the end
products formed by the colonic bacterial action. The mucus protects the colonic
mucosa from the interluminal contents and also provides adherence for the fecal
mass.Slow, weak peristaltic activity moves the colonic contents slowly along
the tract. This slow transport allows efficient reabsorption of water and
electrolytes, which is the primary purpose of the colon. Intermittent strong
peristaltic waves propel the contents for con-siderable distances. This
generally occurs after another meal is eaten, when intestine-stimulating
hormones are released. The waste materials from a meal eventually reach and
distend the rectum, usually in about 12 hours. As much as one fourth of the
waste ma-terials from a meal may still be in the rectum 3 days after the meal
was ingested.
Waste Products of Digestion
Feces
consist of undigested foodstuffs, inorganic materials, water, and bacteria.
Fecal matter is about 75% fluid and 25% solid ma-terial. The composition is
relatively unaffected by alterations in diet, because a large portion of the
fecal mass is of nondietary ori-gin, derived from the secretions of the GI
tract. The brown color of the feces results from the breakdown of bile by the
intestinal bacteria. Chemicals formed by intestinal bacteria (especially indole
and skatole) are responsible in large part for the fecal odor. Gases formed
contain methane, hydrogen sulfide, and ammonia, among others. The GI tract
normally contains approximately 150 mL of these gases, which are either
absorbed into the portal circulation and detoxified by the liver or expelled
from the rectum as flatus.
Elimination
of stool begins with distention of the rectum, which reflexively initiates
contractions of the rectal musculature and relaxes the normally closed internal
anal sphincter. The in-ternal sphincter is controlled by the autonomic nervous
system; the external sphincter is under the conscious control of the cere-bral
cortex. During defecation, the external anal sphincter volun-tarily relaxes to
allow colonic contents to be expelled. Normally, the external anal sphincter is
maintained in a state of tonic con-traction. Thus, defecation is seen to be a
spinal reflex (involving the parasympathetic nerve fibers) that can be
inhibited voluntarily by keeping the external anal sphincter closed.
Contracting the ab-dominal muscles (straining) facilitates emptying of the
colon. The average frequency of defecation in humans is once daily, but the
frequency varies among individuals.
Related Topics