Chapter: Medical Surgical Nursing: Assessment of Digestive and Gastrointestinal Function
Assessment of Digestive and Gastrointestinal Function
Assessment
HEALTH HISTORY AND CLINICAL MANIFESTATIONS
The
nurse begins by taking a complete history, focusing on symp-toms common to GI
dysfunction. These symptoms include pain, indigestion, intestinal gas, nausea
and vomiting, hematemesis, and changes in bowel habits and stool
characteristics. Informa-tion about any previous GI disease is important. The
nurse notes past and current medication use and any previous treatment or
surgery. Information pertaining to medications is of particular in-terest
because medications are a frequent cause of GI symptoms. The nurse takes a
dietary history to assess nutritional status. Ques-tioning about the use of
tobacco and alcohol includes details about type and amount. The nurse and
patient discuss changes in appetite or eating patterns and any examples of
unexplained weight gain or loss over the past year. The nurse also assesses the
stool characteristics. The nurse records all abnormal findings and reports them
to the physician. It is important to include in the history questions about
psychosocial, spiritual, or cultural factors that may be affecting the patient.
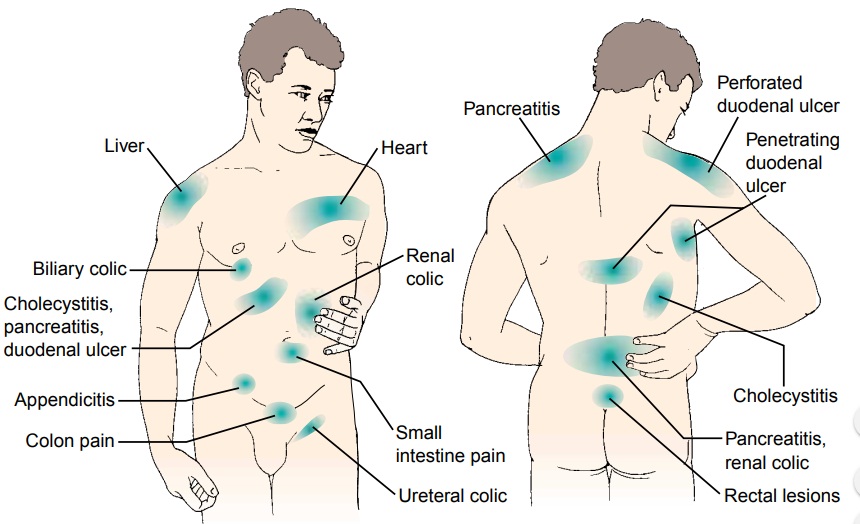
Pain
Pain
can be a major symptom of GI disease. The character, dura-tion, pattern,
frequency, location, distribution of referred pain (Fig. 34-3), and time of the
pain vary greatly depending on the underlying cause. Other factors, such as
meals, rest, defecation, and vascular disorders, may directly affect this pain.
Indigestion
Upper abdominal discomfort or distress associated with eating (commonly called indigestion) is the most common symptom of patients with GI dysfunction. The basis for this abdominal dis-tress may be the patient’s own gastric peristaltic movements. Bowel movements may or may not relieve the pain. Indigestion can result from disturbed nervous system control of the stomach or from a disorder in the GI tract or elsewhere in the body.
Fatty foods tend to
cause the most discomfort, because they remain in the stomach longer than
proteins or carbohydrates do. Coarse vegetables and highly seasoned foods can
also cause considerable distress.
Intestinal Gas
The
accumulation of gas in the GI tract may result in belching (the expulsion of
gas from the stomach through the mouth) or flatu-lence (the expulsion of gas
from the rectum). It is through belch-ing that swallowed air is expelled
quickly when it reaches the stomach. Usually, gases in the small intestine pass
into the colon and are released as flatus. Patients often complain of bloating,
dis-tention, or being “full of gas.” Excessive flatulence may be a symp-tom of
gallbladder disease or food intolerance.
Nausea and Vomiting
Vomiting
is another major symptom of GI disease. Vomiting is usually preceded by nausea,
which can be triggered by odors, ac-tivity, or food intake. The emesis, or
vomitus, may vary in color and content. It may contain undigested food
particles or blood (hematemesis). When vomiting occurs soon after hemorrhage,
the emesis is bright red. If blood has been retained in the stom-ach, it takes
on a coffee-ground appearance because of the action of the digestive enzymes.
Change in Bowel Habits and Stool Characteristics
Changes
in bowel habits may signal colon disease. Diarrhea (an abnormal increase in the
frequency and liquidity of the stool or in daily stool weight or volume)
commonly occurs when the contents move so rapidly through the intestine and
colon that there is in-adequate time for the GI secretions to be absorbed.
Diarrhea is sometimes associated with abdominal pain or cramping and nau-sea or
vomiting. Constipation (a decrease in the frequency of stool, or stools that
are hard, dry, and of smaller volume than normal) may be associated with anal
discomfort and rectal bleeding.
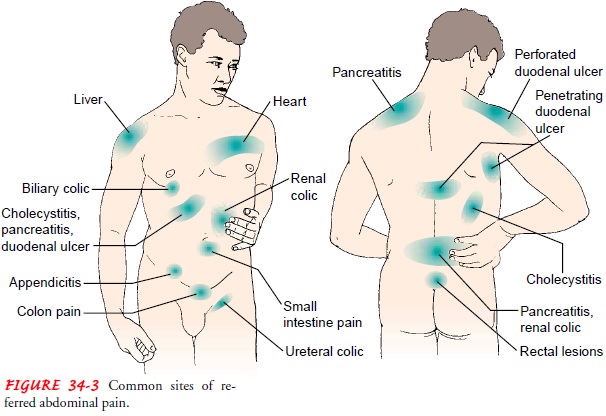
The
characteristics of the stool can vary greatly. Stool is nor-mally light to dark
brown. However, many circumstances, includ-ing the ingestion of certain foods
and medications, can change the appearance of stool (Table 34-3). Blood in the
stool can present in various ways and must be investigated. If blood is shed in
sufficient quantities into the upper GI tract, it produces a tarry-black
color (melena). Blood entering the lower
portion of the GI tract or pass-ing rapidly through it will appear bright or
dark red. Lower rectal or anal bleeding is suspected if there is streaking of
blood on the surface of the stool or if blood is noted on toilet tissue. Other
com-mon abnormalities in stool characteristics that the patient may de-scribe
during the health history include the following:
•
Bulky, greasy, foamy stools that are foul in odor;
stool color is gray, with a silvery sheen
•
Light gray or clay-colored stool, caused by the
absence of urobilin
•
Stool with mucus threads or pus that may be visible
on gross inspection of the stool
•
Small, dry, rock-hard masses called scybala;
sometimes streaked with blood from rectal trauma as they pass through the
rectum
•
Loose, watery stool that may or may not be streaked
with blood
PHYSICAL ASSESSMENT
The
physical examination includes assessment of the mouth, ab-domen, and rectum.
The mouth, tongue, buccal mucosa, teeth, and gums are inspected, and ulcers,
nodules, swelling, discol-oration, and inflammation are noted. People with
dentures should remove them during this part of the examination to allow good
visualization.
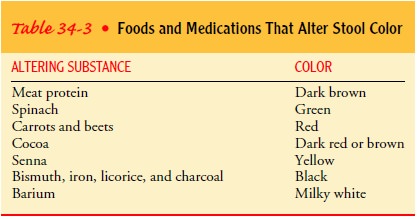
The
patient lies supine with knees flexed slightly for inspec-tion, auscultation,
palpation, and percussion of the abdomen (Fig. 34-4). The nurse performs
inspection first, noting skin changes and scars from previous surgery. It also
is important to note the contour and symmetry of the abdomen, to identify any
localized bulging, distention, or peristaltic waves.
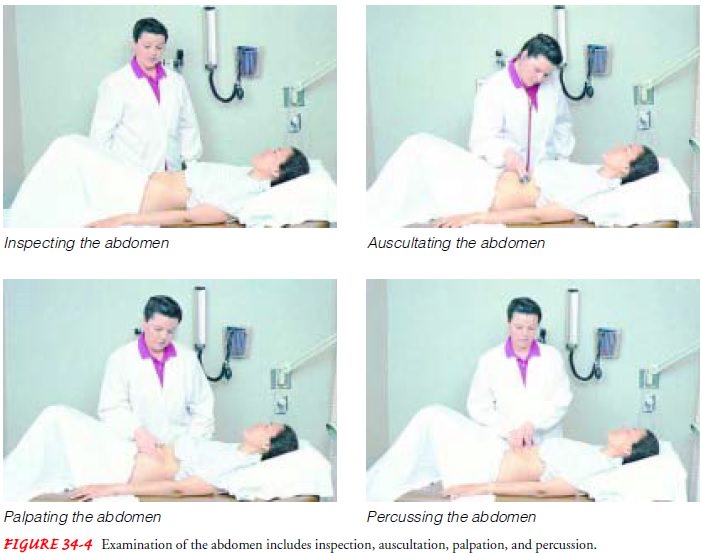
The
nurse performs auscultation before percussion and palpa-tion (which can
increase intestinal motility and thereby change bowel sounds) and notes the
character, location, and frequency of bowel sounds. The nurse assesses bowel
sounds in all four quad-rants using the diaphragm of the stethoscope; the
high-pitched and gurgling sounds can be heard best in this manner. It is
im-portant to document the frequency of the sounds, using the terms normal (sounds heard about every 5 to 20
seconds), hypoactive (one or two
sounds in 2 minutes), hyperactive (5
to 6 sounds heard in less than 30 seconds), or absent (no sounds in 3 to 5 minutes).
The
nurse notes tympany or dullness during percussion. Use of light palpation is
appropriate for identifying areas of tender-ness or swelling; the nurse may use
deep palpation to identify masses in any of the four quadrants. If the patient
identifies any area of discomfort, the nurse can assess for rebound tenderness.
To elicit rebound tenderness, the nurse exerts pressure over the area and then
releases it quickly. It is important to note any pain experienced on withdrawal
of the pressure. The nurse notes any abnormal finding in relation to the
surface landmarks (xiphoid process, costal margins, anterior iliac spine, and
symphysis pubis) or in relation to the four quadrants commonly used to describe
the abdomen (right upper quadrant, RUQ; right lower quadrant, RLQ; left upper
quadrant, LUQ; and left lower quadrant, LLQ) (Bickley & Hoekelman, 1999).
The final part of the examination is inspection of the anal and perineal area. The nurse should inspect and palpate areas of ex-coriation or rash, fissures or fistula openings, or external hemor-rhoids. A digital rectal examination can be performed to note any areas of tenderness or mass.
Related Topics