Chapter: Medicine Study Notes : Musculo-Skeletal
Fractures
Fractures
Management of Fracture of the extremities
·
Immediate assessment:
o Straighten any displaced fracture to allow adequate blood flow
o Examine for fractures
o Examine for dislocations
o Compartment syndromes
o Look for vascular injuries: Hard to assess for vascular injuries when SBP
is less than 90 mm Hg
o Look for nerve injuries
·
Goals of fracture management:
o Upper limb: restore function
o Lower limb: obtain and maintain alignment ® restore
alignment, angulation, rotation and length
·
Principles:
o Reduce severe deformity as soon as possible if it is causing soft-tissue or neurovascular compromise
o Open fractures ® antibiotics
o Assess for conservative or surgical treatment
o Management is a tension between immobilising it long enough to enable
union, and short enough to stop stiffening/arthritis of immobilised joints
· Methods:
o Immobilise. However, casting ® muscle
atrophy, stiff joints, OA, DVT
o Reduction: by manipulation, traction or open reduction
o If it involves joint articulations: open reduction and fixation
(especially if displaced) so that early movement can occur, otherwise secondary
OA
o Internal fixation: plates, nails (Kuntscher) or wires (Kirschner)
o External fixation: screws into bone with external bracing
·
Rules for manipulation to obtain
closed reduction:
o If you manipulate, then re-xray now
o Review early (eg after 1 week).
Can‟t re-manipulate after this should that be necessary
· Indications for surgery:
o Failure to obtain or maintain closed reduction, or where closed reduction has high failure rate (eg fractured neck of femur)
o Intra-articular fracture (especially if > 1mm displacement after reduction). Failure to operate leads to:
§ Short term: irritant effect of synovial fluid ®
non-union
§ Long term: pain, arthritis, instability
o Arterial compromise
o Open fracture
o Pathological fracture
o Multiple injuries
o Segmental fracture
· Risks of surgery:
o ÂSoft
tissue damage
o ÂŻWound
healing
o Anaesthetic risks
o But potentially quicker recovery
Healing of Fractures
·
Stress fractures occur in:
o The elderly with osteoporosis
o Metabolic bone disease
o Very active runners/sports people (eg tennis, squash)
o Never in kids
·
Factors improving remodelling:
o Young age
o Long bones (for example, cf carpal bones)
o Close to growth plate
o If angle is in the principle direction of movement (ie posterior or
anterior angulation of the radius, given this is in line with flexion and
extension of the wrist)
·
Factors impairing healing:
o Movement
o Non-union
o Infection
o Poor blood supply
o Comminuted
·
Rule of thumb for fracture
healing:
o Upper limb: 4 – 6 weeks (kids at shorter end, adults at longer end, etc)
o Ankle: 6 weeks (close to a joint so want to mobilise early)
o Tibia and femur: up to 12 weeks
o Other specific times for some fractures
·
When to mobilise:
o Stable fractures should be mobilised soon
o Unstable fractures should be stabilised before mobilising
·
Patient advice:
o If the limb distal to a cast ever goes blue, becomes painful or tingles,
elevate it for ½ an hour and if no improvement return immediately (not the next
day). Remove cast and assess for improvement. If no improvement then urgent
opinion
Complications of Fractures
·
Joint stiffness: Cartilage
requires motion for nutrition. If held in one position ® risk of
cartilage deterioration
·
Delayed Union:
o Presents as pain + movement at fracture site with stress
o Normal union times
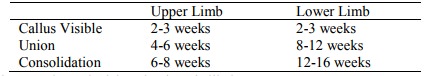
o If these times prolonged “delayed union” is likely
o Causes: Severe soft tissue damage, inadequate blood supply, infection, insufficient splintage, excessive traction
o Clinically: site tender, painful if subjected to stress, x-rays still show visible line
o Treatment: needs to be reviewed if no bridging callus by 3 months. Need
internal fixation and bone grafting
·
Non Union:
o Non-union is likely if delayed union is not treated
o Presents as non-painful movement at the fracture site
o Causes: Too large a gap (bone missing, muscle in way), interposition of periosteum
o Clinical: Painless movement at fracture site. Xray shows smooth and sclerosed bone ends or excessive bone formation
o Treatment: Not all cases need treating eg scaphoid, otherwise fixation
and bone grafting necessary.
·
Infection in open fractures:
o ® Osteomyelitis, slow union and increased chance of refracture
o Clinical: History of open fracture or operation on closed fracture. Wound inflamed. Systemic signs of fever
o Treatment: All open fractures require prophylactic antibiotics and
excision of devitalised tissue. If acutely infected, surrounding tissues should
be opened and drained + antibiotics.
·
Malunion:
o When bone fractures join in an unsatisfactory position i.e. unacceptable
angulation, rotation or shortening
o Aetiology:
§ Failure to reduce a fracture adequately
§ Failure to hold reduction while healing proceeds
§ Gradual collapse of comminuted or osteoporotic bone
o Signs and symptoms: Usually obvious eg. Unusual bone alignment, x-ray
o Treatment:
§ If detected before union complete angulation may be corrected by wedging
of plaster
§ Forcible manipulation under anaesthetic
§ Osteotomy if union complete and deformity severe
·
Compartment Syndrome:
o Elevated pressure in an enclosed space (eg muscle compartment) can
irreversibly damage the contents of that space (eg ischaemia)
o Major causes: Processes constricting the compartment or increasing the
contents of the space:
§ Compressive bandages
§ Tight cast
§ Haemorrhage and oedema after fracture
§ Closure of fascical defects
o Muscles once infarcted are replaced by inelastic fibrous tissue (eg Volkmann‟s Ischaemic
o Contracture of the forearm compartment after humeral supracondylar fracture). Most sensitive test is passive extension of the muscles. Can still have arterial flow through the compartment while muscles are becoming ischaemic
o Signs and symptoms (The 5 p‟s i.e.):
§ Pain
§ Paraesthesia
§ Pallor
§ Pulselessness
§ Paralysis
o Diagnosis: Pressure > 30 – 40mmHg (using needle manometer etc) and/or MRI
o Treatment: Remove bandages, etc, consider decompression with a
fasciotomy if pressure high, with wound left open for 5 days
·
Avascular Necrosis:
o Aetiology
§ Rare
§ Focal subchondral infarction ® collapse of necrotic segment ® joint
deformity ® arthritis
§ Common in bones that derive most of their blood supply from the
medullary cavity
§ Mainly femoral head, also knee, scaphoid, head of talus
§ Gross: infarct is yellow, opaque and chalky with rim of hyperaemic
fibrous tissue
o Causes:
§ Trauma (eg subcapital fractured neck of femur)
§ Secondary to corticosteroid treatment
§ Nitrogen embolisation in divers (® Bends ® Caisson
disease)
§ Sickle cell disease
§ Alcoholism
§ SLE
§ Infective endocarditis
§ Radiation
§ Diabetes mellitus
o Signs and symptoms:
§ Joint stiffness
§ Pain in or near joint
§ Local tenderness
§ Restricted movement
·
Other complications of fractures:
o Venous thromboembolism: injury patients are at risk due to immobility,
leg injury, etc
o Skin necrosis
o Pressure sores
o Fat embolism: typically day 3 – 10. Confusion, sudden SOB, hypoxia.
Immediate ICU management
·
Charcot‟s Joint = neuropathic
joint:
o Causes: diabetic neuropathy, tabes dorsalis, cauda equina, leprosy
o Gross disorganisation of the joints (even dislocation) following
repeated minor trauma ® recurrent stress fractures that aren‟t felt due to neuropathy
Related Topics