Chapter: Medicine and surgery: Cardiovascular system
FallotŌĆÖs tetralogy - Congenital heart disease
FallotŌĆÖs tetralogy
Definition
┬Ę A congenital defect (see Fig. 2.20) of the heart in which there is
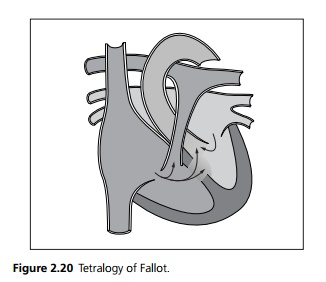
┬Ę A large membranous ventricular septal defect (VSD). Wrongly positioned aorta above the VSD (over ridingaorta).
┬Ę Right ventricular outflow obstruction (pulmonary stenosis).
┬Ę Right ventricular hypertrophy.
Aetiology
Embryological hypoplasia of the conus, which gives rise to the membranous ventricular septum. Occurs in Down syndrome and as part of fetal alcohol syndrome.
Pathophysiology
The pulmonary stenosis results in high right ventricular pressure and hence right ventricular hypertrophy. The large VSD and high right heart pressures cause a right to left shunt. The aorta is over the shunt as the VSD is high and thus there is also flow from the right ventricle directly into the aorta. The degree of pulmonary stenosis is variable (ranging from mild to atresia), thus the clinical picture ranges in severity. The right ventricular outflow tract obstruction is often progressive.
Clinical features
In rare severe cases cyanosis develops within days as the pulmonary circulation is dependent on a patent ductus arteriosus. More commonly presentation is later with progressive cyanosis over a few weeks. Initially it may only be present on exertion, but as the right ventricular outflow obstruction is progressive cyanosis becomes evident at rest, and the characteristic squatting position may be adopted. Squatting traps unsaturated blood in the legs and increases systemic vascular resistance. This reduces the right to left intracardiac shunt and provides some symptomatic relief. On examination cyanosis and clubbing may be present. There is a right ventricular heave. On auscultation there is initially a long systolic murmur across the pulmonary valve, which shortens as cyanosis develops.
Spasm of the infundibular muscle in the right ventricular outflow tract results in further compromises the right cardiac outflow causing worsening cyanosis and often loss of consciousness. These are termed hypercyanotic or tet spells.
Investigations
Chest X-ray often shows a heart of normal size but the left heart border is concave (boot shape) due to the small pulmonary trunk. There is normally pulmonary oligaemia due to low pulmonary blood flow. ECG shows right axis deviation and right ventricular hypertrophy. Echocar-diogram is diagnostic.
Management
Symptomatic infants may require a BlalockŌĆōTaussig shunt, using a tube of Gortex to connect the subclavian artery to the pulmonary artery. This provides a left to right shunt replacing the duct as it closes.
Surgical correction is performed at 4ŌĆō6 months under cardiopulmonary bypass. It is performed by opening the pulmonary stenosis (by patch enlargement where indicated) and closure of the VSD.
Related Topics