Chapter: Basic Radiology : Plain Film of the Abdomen
Exercise: Extraluminal Gas Pattern
EXERCISE 8-6.
EXTRALUMINAL GAS PATTERN
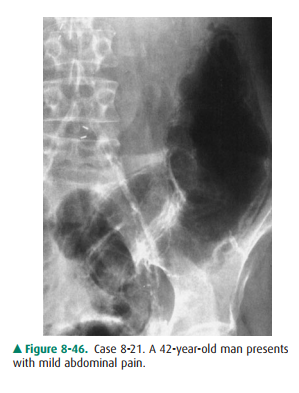
8-21. What is the most
likely diagnosis in Case 8-21 (Figure8-46)?
A.
Colonic diverticulitis
B.
Mechanical obstruction of the colon
C.
Pneumatosis cystoides intestinalis
D.
Pneumoperitoneum
8-22. What is the most
likely diagnosis in Case 8-22 (Figure8-47)?

A.
Abscess
B.
Functional ileus
C.
Gallstone ileus with gas in the biliary tree
D.
Hepatic portal vein gas
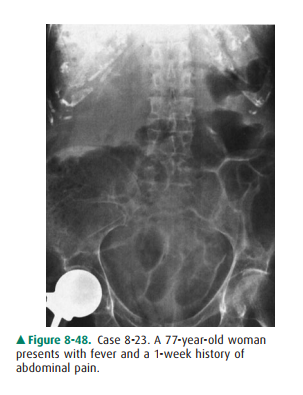
8-23. What is the most
likely diagnosis in Case 8-23 (Figure8-48)?
A.
Gallstone ileus with gas in the biliary tree
B.
Hepatic portal venous gas
C.
Pneumoperitoneum
D.
Right subdiaphragmatic abscess.
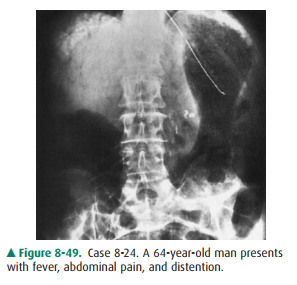
8-24. What is the most
likely diagnosis in Case 8-24 (Figure8-49)?
A.
Gallstone ileus with gas in the biliary tree
B.
Hepatic portal venous gas
C.
Pneumoperitoneum
D.
Subdiaphragmatic abscess
Radiologic Findings
8-21. This case shows
linear air streaks along the descend-ing and sigmoid colon in a patient with
mild ab-dominal pain. These streaks indicate pneumatosis cystoides intestinalis
(C is the correct answer to Question 8-21).
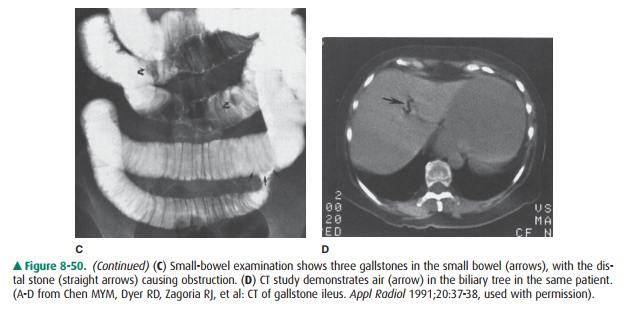
8-22. This case shows a
distended proximal jejunum and a few air bubbles in the right upper quadrant,
indicat-ing gallstone ileus with mechanical obstruction and air in the biliary
tree (Figure 8-50 A). An upper gas-trointestinal study demonstrates a distended
proximal small bowel, a fistula (Figure 8-50B) between the bil-iary tree and
the duodenum, and three gallstones in the small bowel (Figure 8-50 C). CT shows
air in the biliary tree (Figure 8-50 D) (C is the correct answer to Question
8-22).
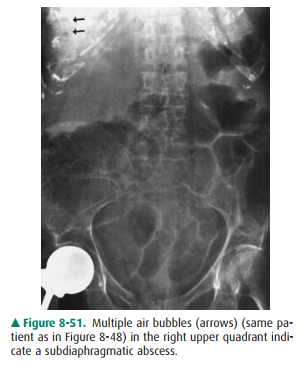
8-23. In this case,
multiple air bubbles in the right upper quadrant in a patient with fever are
consistent withsubdiaphragmatic abscess (Figure 8-51). Bilateral linear rib
calcifications and right hip replacement are also seen (D is the correct answer
to Question 8-23).
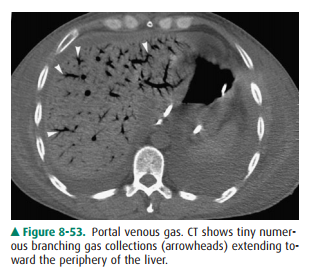
8-24. This case shows a
fine arborizing linear gas pattern in the right upper quadrant extends to the
periphery of the liver, indicating portal venous gas (B is correct answer to
Question 8-24).
Discussion
Pneumatosis cystoides
intestinalis appears as linear streaks of gas or intramural cystic collections
of gas in the small bowel or colon. The cysts range in size from 0.5 to 3 cm
and may extend into the adjacent mesentery. Pneumatosis intestinalis is an
incidental finding in most patients, usually with a self-limited benign course;
simple bowel obstruction, volvulus, and air from the mediastinum or
retroperitoneum are commonly associated. Pneumatosis intestinalis may be caused
by ischemic and necrotizing enterocolitis in patients with leukemia or
non-Hodgkin lymphoma and in those who have had bone marrow transplantation.
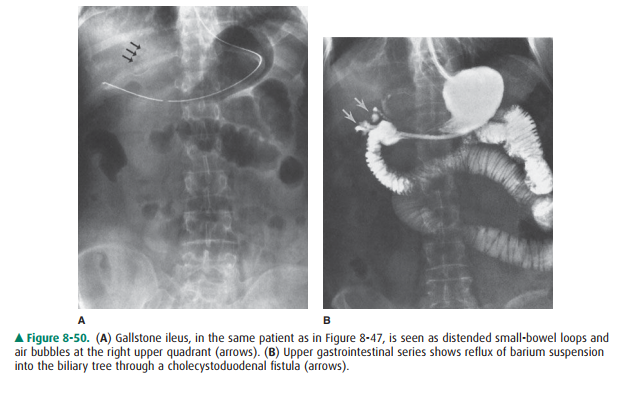
Gallstone ileus, the mechanical
obstruction of the small bowel by an impacted gallstone, is commonly seen in
elderly women. Clinical presentation in gallstone ileus is nonspecific, and the
mortality rate is high (15%). A gallstone enters the intestinal lumen via a
cholecystoenteric fistula. Major radi-ographic signs include small-bowel obstruction,
air in the biliary tree, and an ectopic gallstone seen on plain abdominal film,
upper gastrointestinal series, or CT study.
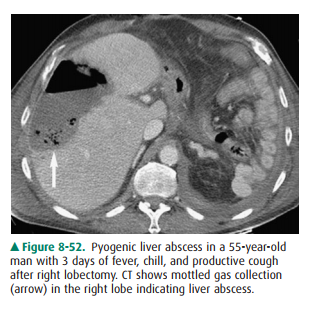
Abscess in the subphrenic and
subhepatic spaces is a se-rious problem, with a mortality rate of 30%.
Subphrenic abscess may arise spontaneously or as a complication of ab-dominal
surgery, pancreatitis, diverticulitis, or appendicitis. A cluster of gas may be
seen on plain film in 70% of abscesses. Left-sided abscess is difficult to
discern because gas in the splenic flexure, stomach, or jejunum may mimic gas
within the abscess. Other radiographic findings include elevation of the
adjacent hemidiaphragm, pleural effusion, and basilar at-electasis. CT is more
accurate in assessing hepatic and extra-hepatic abscess (Figure 8-52).
In the right upper quadrant, when
multiple tubular lu-cencies are seen reaching the lateral hepatic margins,
portal venous gas is a likely consideration (Figure 8-53). Biliary tree gas is
located in the central hepatic zone near the porta he-patis. Benign portal
venous gas has been noted in sigmoid diverticulosis, nonobstructed splenic
flexure carcinoma, ul-cerative colitis, and bronchopneumonia. Mesenteric
vascular insufficiency and necrotizing intestinal infection are common causes
of hepatic portal venous gas. In children, necrotizing enterocolitis produces
intramural gas within mesenteric veins to the liver; the mortality rate in
patients with the sign of hepatic portal venous gas is higher than in those
without portal venous gas.
Related Topics