Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Perioperative Pain Management & Enhanced Outcomes
Evolution of Enhanced Recovery Programs
Evolution of Enhanced Recovery Programs
Despite increasing numbers of surgical patients who present with complex
surgical problems and numerous medical comorbidities, major advances in
surgical and anesthetic management have pro-gressively decreased perioperative
mortality and morbidity. Further improvement in perioperative outcomes,
highlighted by accelerated postopera-tive convalescence and decreasing
occurrence of perioperative complications, will depend on con-tinued evolution
of an integrated, multidisciplinary team approach to perioperative care that
requires adjustments in multiple aspects of care, including surgical and
anesthetic techniques, nursing care, physiotherapy, and nutrition support. The
goal is to combine individual evidence-based elements of perioperative care,
each of which may have modest benefits when used in isolation, into a tightly
coor-dinated effort that has a synergistic, beneficial effect on surgical outcomes.
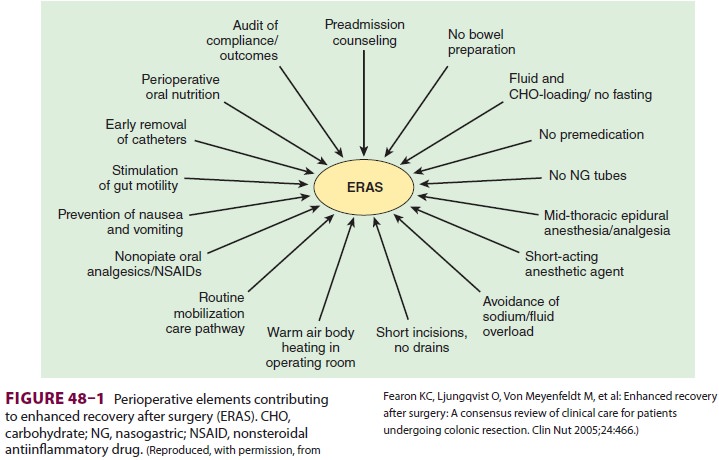
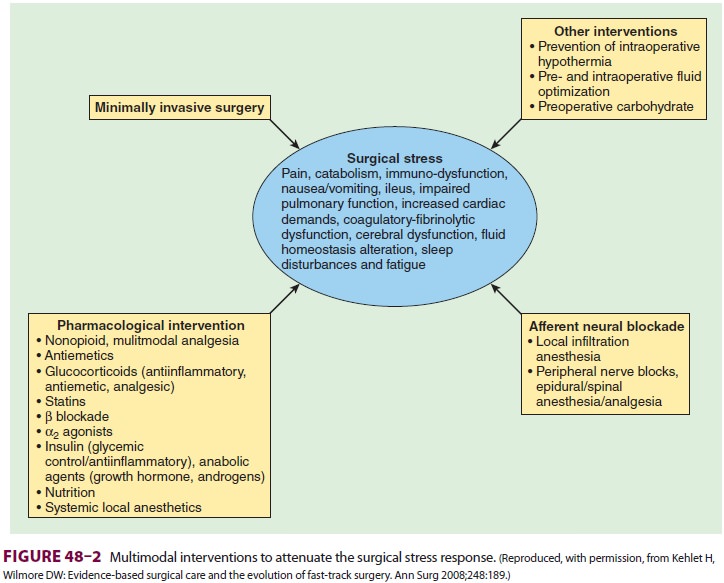
Such coordinated, multidisciplinary
periopera-tive care programs are termed enhanced
recovery pro-grams (ERPs), fast-track
surgery, or enhanced recovery after surgery (ERAS) (Figure 48–1). A
well-functioning ERP uses evidence-based practices to decrease variation in
clinical management, minimize organ dysfunction, and accelerate conva-lescence
(Figure 48–2). Although many publications in the surgical literature have
highlighted the positive impact of such programs on surgical outcomes, reports
documenting the role of anesthesia and anal-gesia in these programs are few.
Another challenge is determining how to assess the impact of anesthetic
management on outcomes in an ERP. Hospital length of stay is the most commonly
used measure of suc-cess, but in many systems timing of hospital dis-charge is
more directly related to administrative and
organizational issues than to discrete milestones in the patient’s
postoperative recovery. Little research has been undertaken to define the
process of postop-erative recovery, and few outcome measures are currently
available to confirm that postoperative recovery has been accomplished for a
given surgical disease. Other measures of successful implementa-tion of ERPs
are reduced readmission and complica-tion rates.
It is logical to assume that more effective anes-thetic interventions
will reduce pain, facilitate ear-lier postoperative mobilization, and allow
earlier resumption of oral feeding. In this context, the role of the anesthesia
provider must evolve from merely providing satisfactory anesthetic conditions
throughout the operation to a focus on enhancing overall perioperative care
through techniques that shorten postoperative convalescence and reduce the
likelihood of perioperative complications. These goals can be achieved by
optimizing the patient’s preoperative condition, by ablating the adverseeffects
of the intraoperative neuroendocrine stress response, and by providing pain and
symptom control to facilitate the postoperative recovery. In endeavoring to do
so, the anesthesiologist must become a perioperative physician and an active
par-ticipant in the surgical team.
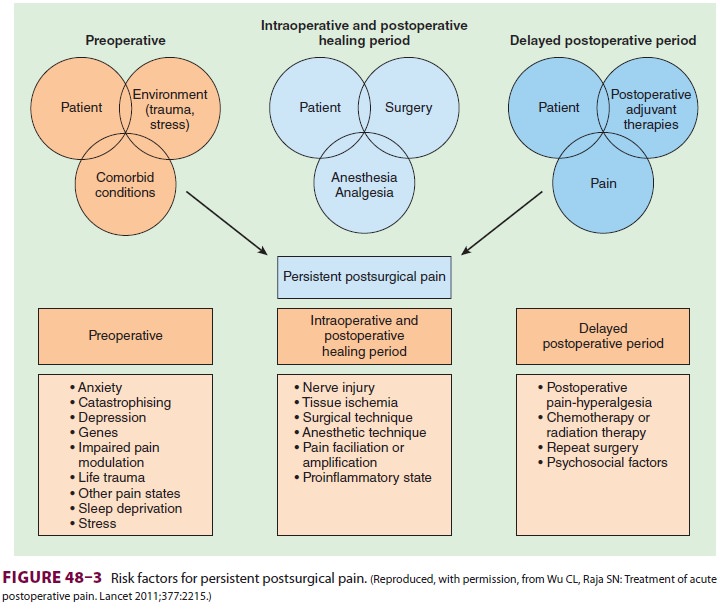
The problem of persistent postsurgical pain,
defined as chronic pain that continues beyond the typical healing period of 1–2
months following surgery—or well past the normal period for
post-operative follow-up by anesthesia providers—is increasingly acknowledged
as a common and sig-nificant issue following surgery. The incidence of
persistent postsurgical pain may exceed 30% after some operations, especially
amputations, thora-cotomy, mastectomy, and inguinal herniorrha-phy. Although
the cause is unclear, several risk factors have been identified ( Figure 48–3), and aggressive, multimodal
perioperative pain control is often suggested as a fundamental preemptive
strategy.
Related Topics