Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Perioperative Pain Management & Enhanced Outcomes
Anesthetic Management: Postoperative Period
POSTOPERATIVE PERIOD
Immediate Postoperative Care
A. Strategies to Minimize Postoperative Shivering
The primary cause of postoperative shivering
is perioperative hypothermia, although other, non-thermoregulatory, mechanisms
may be involved. Postoperative shivering can greatly increase oxygen
consumption, catecholamine release, cardiac out-put, heart rate and blood
pressure, and intracerebral and intraocular pressure. It increases
cardiovas-cular morbidity, especially in elderly patients, and increases length
of stay in the postanesthesia care unit. Shivering is uncommon in elderly and
hypoxic patients: the efficacy of thermoregulation decreases with aging, and
hypoxia can directly inhibit shiver-ing. Many drugs, notably meperidine,
clonidine, and tramadol, can be used to reduce postoperative shiv-ering; however,
prevention of hypothermia is the most efficient strategy.
B. PONV Treatment
Pharmacological treatment of PONV should be promptly initiated once
medical or surgical causes of PONV have been ruled out. PONV and its treat-ment
are reviewed.
C. Multimodal Analgesia
The scientific rationale for multimodal
analgesia is to combine different classes ofmedications, having different
(multimodal) phar-macological mechanisms of action and additive or synergistic
effects, to control multiple periopera-tive pathophysiological factors that
lead to postop-erative pain and its sequelae. Such an approach may achieve
desired analgesic effects while reduc-ing analgesic dosage and associated side
effects, and often includes utilization of regional analgesic techniques such as
local anesthetic wound infu-sion, epidural or intrathecal analgesia, or
single-shot or continuous peripheral nerve blockade. Multimodal analgesia is
routinely utilized in ERPs to improve postoperative outcomes. Discus-sion here focuses on
the principal analgesicinterventions that can be used in perioperative
multimodal analgesia regimens.
1. NSAIDs—The addition of nonsteroidal antiinflammatory drugs (NSAIDs) to systemicopioids diminishes postoperative pain intensity, reduces the opioid requirement by approximately 30%, and decreases opioid-related side effects such as PONV and sedation. However, NSAIDs may increase the risk of gastrointestinal and postopera-tive bleeding, decrease kidney function, increase the risk of anastomotic leakage after colorectal surgery, and impair wound healing.
Perioperative administration of
cyclooxygen-ase-2 (COX-2) inhibitors likewise reduces postop-erative pain and
decreases both opioid consumption and opioid-related side effects, and while
their use has reduced the incidence of NSAID-related plate-let dysfunction and
gastrointestinal bleeding, the adverse effects of COX-2 inhibitors on kidney
func-tion remain controversial. Concerns have also been raised regarding their
safety for patients undergoing cardiovascular surgery; these have centered on
rofe-coxib and valdecoxib, specifically. Increased cardio-vascular risk
associated with the perioperative use of celecoxib or valdecoxib in patients
with minimal cardiovascular risk factors and undergoing nonvas-cular surgery
has not been proven. Further studies are needed to establish the analgesic
efficacy and safety of COX-2 inhibitors and their clinical effect on
postoperative outcomes.
2. Acetaminophen
(paracetamol)—Oral, rectal,and parenteral acetaminophen is
a common com-ponent of multimodal analgesia. Acetaminophen’s analgesic effect
is 20–30% less than that of NSAIDs, but its pharmacological profile is safer.
Analgesic efficacy improves when the drug is administered together with NSAIDs,
and it significantly reduces pain intensity and spares opioid consumption after
orthopedic and abdominal surgery. However, acet-aminophen may not reduce
opioid-related side effects. Routine administration of acetaminophen in
combination with regional anesthesia and analgesia techniques may allow NSAIDs
and COX-2 inhibi-tors to be reserved for control of breakthrough pain, thus
limiting the incidence of NSAID-related side effects.
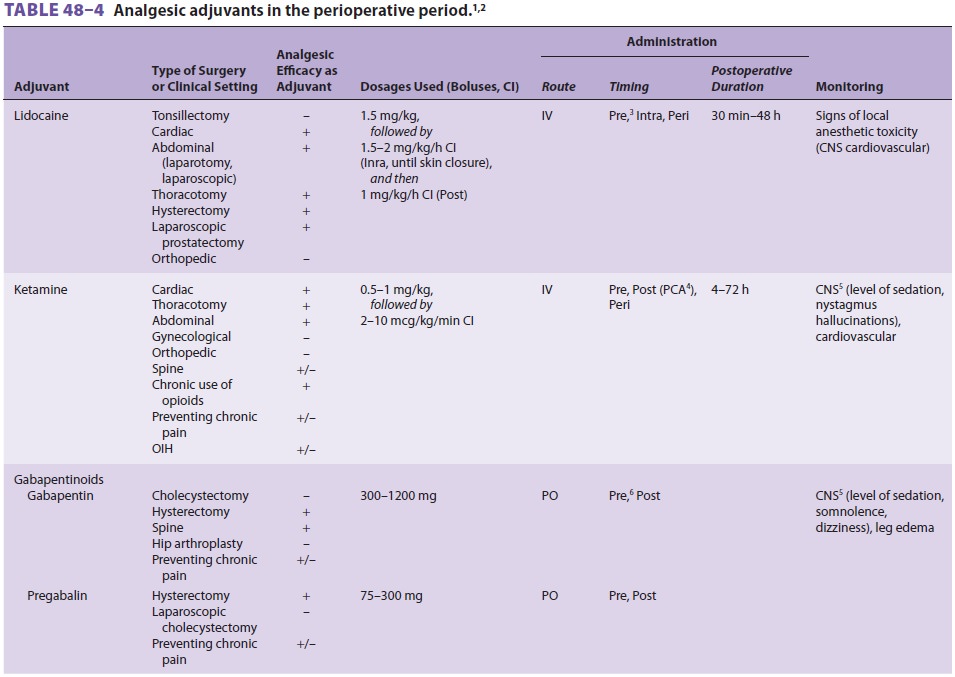
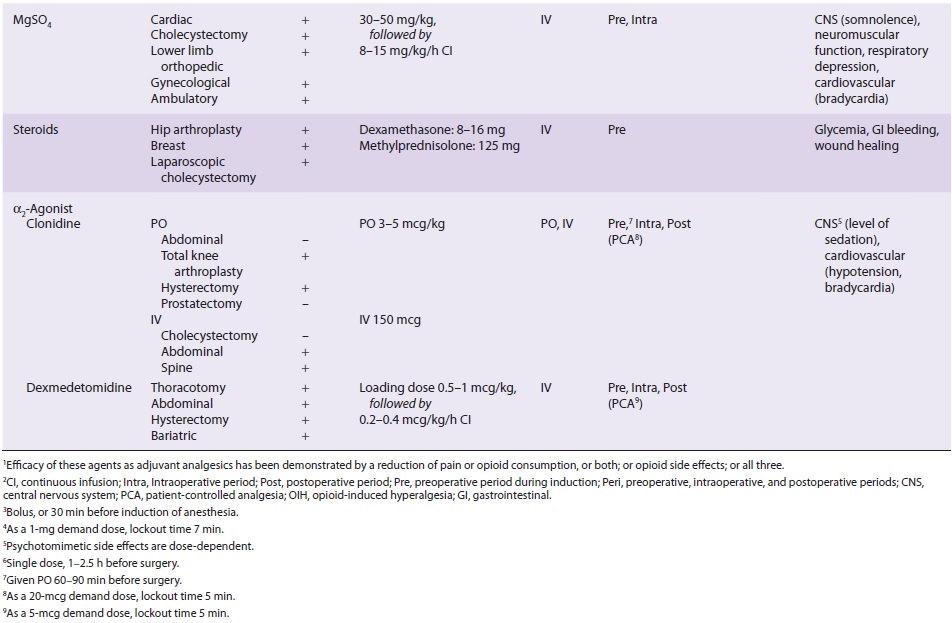
3. Opioids—Despite the increasing use of new, nono-pioid analgesic medications and adjuvants and of regional anesthesia and analgesia techniques intended to minimize opioid requirements and opioid-related side effects (Table 48–4), the use of systemic opioids remains a cornerstone in the management of surgical pain. Parenteral opioids are frequently prescribed in the postoperative period during the transitional phaseto oral analgesia. Opioid administration by patient-controlled analgesia (PCA) provides better pain control, greater patient satisfaction, and fewer opioid side effects when compared with on-request parenteral opioid administration. Oral admin-istration of opioids, such as immediate-release and controlled-release oxycodone or hydromorphone, in combination with NSAIDs or acetaminophen, or both, is commonly used in the perioperative period. Preoperative administration of extended-release oxy-codone in patients undergoing surgery of short dura-tion provides adequate plasma concentration and analgesia following discontinuance of remifentanil infusion. Tramadol, a partial opioid agonist, has beenassociated with an increased incidence of PONV.
4. Epidural analgesia—In addition to providingexcellent analgesia, epidural blockade blunts the stress response associated with surgery, decreases postoperative morbidity, attenuates catabolism, and accelerates postoperative functional recovery. Com-pared with systemic opioid analgesia, thoracic epi-dural analgesia provides better static and dynamic pain relief. Long-acting local anesthetics such as ropivacaine (0.2%), bupivacaine (0.1–0.125%), and levobupivacaine (0.1–0.125%) are commonly administered together with lipophilic opioids by continuous epidural infusion or by patient-con-trolled epidural analgesia (PCEA). Administering low doses of local anesthetic via thoracic epidural infusion avoids lower extremity motor blockade that may delay postoperative mobilization and recovery. Adding fentanyl or sufentanil to epidural local anes-thetics improves the quality of postoperative anal-gesia without delaying recovery of bowel function.
High thoracic epidural analgesia has been intro-duced in patients undergoing cardiac surgery based on data from small randomized clinical trials that suggested benef cial effects on postoperative outcomes. A recent meta-analysis of more than 2700 patients who underwent cardiac surgery and received high thoracic epidural analgesia showed an overall reduction of pulmonary complications (rela-tive risk 0.53) and supraventricular arrhythmias (relative risk 0.68), but no reduction in incidence of myocardial infarction, stroke, or postoperative mortality. Due to concerns about the risk of epidural hematoma and its devastating neurological conse-quences in patients fully heparinized during cardio-pulmonary bypass, the use of high thoracic epidural analgesia is understandably limited.
5. Peripheral nerve block—Single-shot andcontinuous peripheral nerve blockade isfrequently utilized for fast-track ambulatory and inpatient orthopedic surgery, and can accelerate recovery from surgery and improve analgesia and patient satisfaction . The opioid-sparing effect of nerve blocks minimizes the risk of opioid-related side effects. Appropriate patient selection and strict adherence to institutional clini-cal pathways helps ensure the success of peripheral nerve blockade as a fast-track orthopedic analge-sia technique. Peripheral nerve blockade has also been used as a component of multimodal analgesia for abdominal surgery; for example, transverseus abdominis plane (TAP) block in patients undergo-ing total abdominal hysterectomy provides effective analgesia and decreases morphine consumption and sedation when compared with patients receiv-ing morphine alone via PCA.
Local
anesthetic wound infusion—The analgesicefficacy of
local anesthetic wound infusion has been established for multiple surgical
procedures. Incon-sistent results may be due to factors that include type,
concentration, and dose of local anesthetic, catheter placement technique and
type of catheter, mode of local anesthetic delivery, incision location, and
dis-lodgment of the catheter during patient mobilization.
Strategies to Facilitate Recovery on the Surgical Unit
A. Organization of Multidisciplinary Surgical Care
The multidisciplinary aspect of postoperative
care should bring together the surgeon, the nurse, the anesthesiologist, the
nutritionist, and the physio-therapist in an effort to customize individual
patient care based on standardized, procedure-specific protocols. Comfortable
chairs and walkers need to be made readily available near each patient bed to
encourage patients to sit, stand, and walk. The ben-efits of mobilization for
cardiovascular homeostasis and bowel function have been shown repeatedly.
Patients should be encouraged to sit the evening fol-lowing surgery, with
ambulation starting the next day for a minimum of 4–6 h each day. If patients
cannot get out of bed, they should be encouraged to perform physical and deep
breathing exercises.
B. Optimization of Analgesia to Facilitate Functional Recovery
well-organized, well-trained, highly
motivated acute pain service (APS) and surgical nursing work-force, utilizing
procedure-specific clinical proto-cols to optimally manage analgesia and
related side effects, is critically important for fast-track surgery. The
quality of pain relief and symptom control heav-ily influences postoperative
recovery; optimal mobi-lization and dietary intake depend upon adequate
analgesia. The anesthesiologist, in coordination with the APS, must identify
and employ the optimal analgesic techniques tailored to the specific surgical
procedure, and the quality of analgesia and possible presence of side effects
must be closely and con-tinuously assessed. The patient must be comfortable
ambulating and performing physiotherapy, with minimal side effects such as
lightheadedness, seda-tion, nausea and vomiting, and leg weakness.
C. Strategies to Minimize Postoperative Ileus
Postoperative ileus delays
enteral feeding, causes patient
discomfort, and is one of the most
common causes of
prolonged postopera-tive hospital
stay. Because early enteral nutrition is associated with decreased
postoperative morbidity, interventions and strategies aimed at decreasing
postoperative ileus are required for patients in an ERP. Three main mechanisms
contribute to ileus: sympathetic inhibitory reflexes, local inflamma-tion
caused by surgery, and postoperative opioid analgesia. The nasogastric tube,
frequently inserted after abdominal surgery, does not speed the recov-ery of
bowel function and may increase pulmonary morbidity by increasing the incidence
of aspiration. Therefore, nasogastric tubes should be discouraged whenever
possible or used for only a very short period of time, even in gastric and
hepatic surgery.
Multimodal analgesia and nonopioid analgesia
techniques shorten the duration of postoperative ileus. Continuous epidural
local anesthetic infu-sion improves the recovery of bowel function by
suppressing the inhibitory sympathetic spinal cord reflexes. Thoracic epidural
analgesia with local anesthetics and small doses of opioids reduces the
incidence of ileus and improves postoperative pain relief. Minimally invasive
surgery decreases surgical stress and inflammation, resulting in a faster
return of bowel function. Any role of epidural analgesia in accelerating the
recovery of bowel function after laparoscopic surgery remains controversial, at
best. Laxatives, such as milk of magnesia and bisacodyl, reduce postoperative
ileus duration. Prokinetic medications such as metoclopramide are ineffec-tive.
Neostigmine increases peristalsis but may also increase the incidence of PONV.
Excessive perioperative fluid administration
commonly causes bowel mucosal edema and delays postoperative return of bowel
function. However, results from a randomized double-blind study of lib-eral
versus restricted fluid administration showed no differences with regard to
recovery of bowel function in patients undergoing fast-track abdomi-nal
surgery. No studies have compared crystalloid versus colloid administration in
terms of their effecton the
return of bowel function. Because either excessive, or excessively restricted,
perioperative fluid therapy may
increase the incidence and severity of postoperative ileus, a goal-directed
fluid strategy (discussed earlier) should be selected to decrease postoperative
morbidities and enhance recovery and should be utilized according to the type
of surgery and patient comorbidities.
Postoperative chewing gum, by stimulating
gas-trointestinal reflexes, may decrease ileus duration. Although its effect
has not been evaluated in ERP patients, postoperative chewing gum may be
included in multimodal interventions to decrease postopera-tive ileus because
of its safety and low cost. Peripheral opioid μ-receptor antagonists
methylnaltrexone and alvimopan have been introduced to minimize the adverse
effects of opioids on bowel function without antagonizing opioid analgesia. In
patients receiving large-dose intravenous morphine analgesia, alvimo-pan
decreases the duration of postoperative ileus by 16–18 h, the incidence of
nasogastric tube reinser-tion, postoperative morbidity, and hospital length of
stay and readmission rates, especially in patients undergoing bowel resection.
Nevertheless, the recov-ery of bowel function is slower when compared with
patients receiving multimodal strategies in an ERP.
Related Topics