Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Perioperative Pain Management & Enhanced Outcomes
Anesthetic Management: Intraoperative Period
INTRAOPERATIVE PERIOD
Antithrombotic Prophylaxis
Antithrombotic prophylaxis reduces
perioperative venous thromboembolism and related morbidity and mortality. Both
pneumatic compression devices and anticoagulant medications are now commonly
used. Because neuraxial anesthesia techniques are commonly employed for many
patients during major abdominal, vascular, thoracic and orthope-dic surgery,
appropriate timing and administration of antithrombotic agents in these cases
is of critical importance in order to avoid the risk of epidural hematoma.
International recommendations on the management of anticoagulated patients
receiving regional anesthesia have been recently revised and published and are
discussed.
Antibiotic Prophylaxis
Appropriate selection and timing of preoperative antibiotic prophylaxis
reduces the risk of surgi-cal site infections. Antibiotics should be adminis-tered
within 1 h before skin incision and, based on their plasma half-life, should be
repeated during prolonged surgeries to ensure adequate tissue con-centrations.
Antibiotic prophylaxis of surgical site infections should be discontinued
within 24 h after surgery (current guidelines permit cardiothoracic patients to
receive antibiotics for 48 h following surgery).
Strategies to Minimize the Surgical Stress Response
The surgical stress response is characterized
by neu-roendocrine, metabolic, and inflammatory changes initiated by the
surgical incision and subsequent procedures that can adversely affect organ
function and perioperative outcomes, especially in elderly and physiologically
compromised patients. These responses include a transient but reversible state of
insulin resistance, characterized by
decreasedperipheral glucose uptake and increased endogenous glucose production.
The magnitude of the surgical stress response is related to theintensity of the
surgical stimulus; can be amplified by other factors, including hypothermia and
psy-chological stress; and can be moderated by periop-erative interventions,
including deeper planes of general anesthesia, neural blockade, and reduction
in the degree of surgical invasiveness. Much recent effort has focused on
developing surgical and anes-thetic techniques that reduce the surgical stress
response, with the goal of lowering the risk of stress-related organ
dysfunction and perioperative compli-cations. An overview of several techniques
that have proved effective in ERP protocols follows.
A. Minimally Invasive Surgery
Laparoscopic procedures are associated with a reduced incidence of
surgical complications, espe-cially surgical site infections, compared with the
same procedures performed in “open” fashion. Published data highlight the
safety of minimally invasive procedures in the hands of adequately trained and
experienced surgeons. Laparoscopic cholecystectomy results in shorter length of
hos-pital stay and fewer complications compared with open cholecystectomy, and
similar results have been reported for colorectal surgery. A longer
termsalutary impact is achieved when laparoscopic techniques are included in
ERPs. A laparoscopic approach is also associated with less morbidity in elderly
surgical patients.
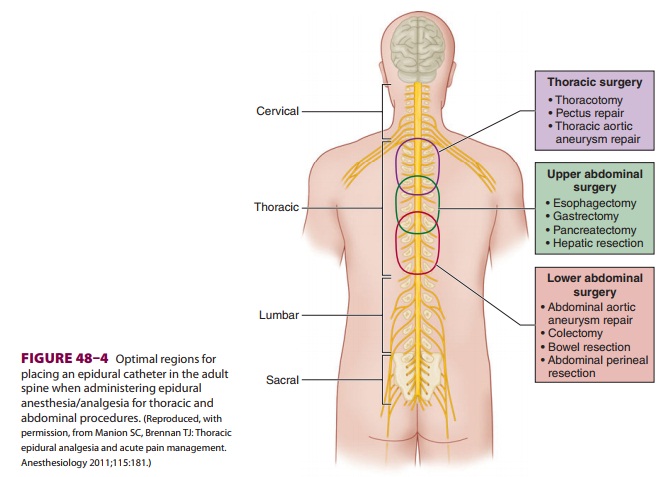
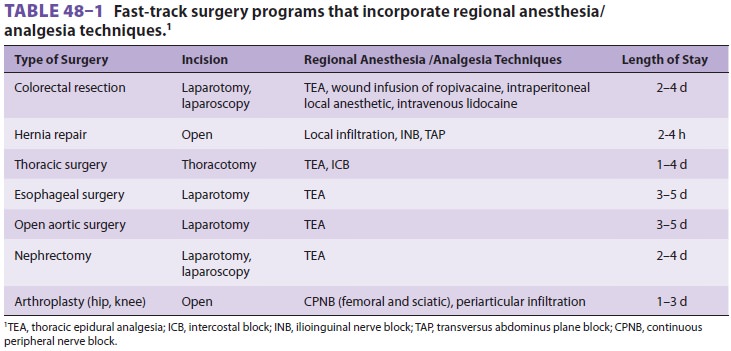
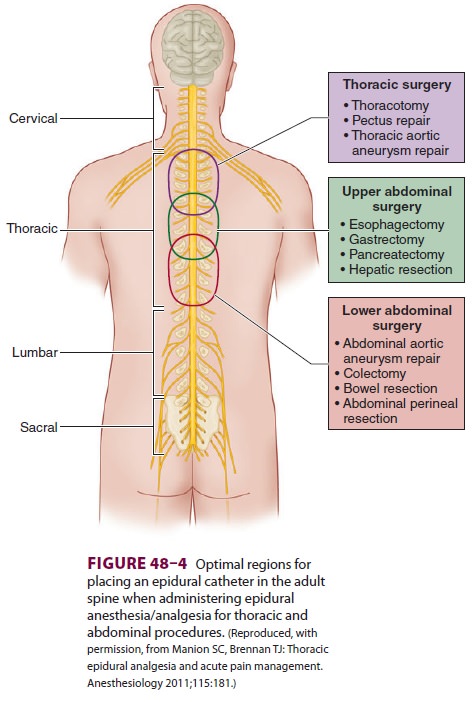
B. Regional Anesthesia/Analgesia Techniques
A variety of fast-track surgical procedures
have taken advantage of the beneficial clinical and metabolic effects of
regional anesthesia/analgesia techniques(Table 48–1). Neuraxial blockade of nocicep-tive stimuli by epidural and spinal
local anesthetics has been shown to blunt the metabolic and neuroendocrine
stress response to surgery. To be effective, the blockade must be established
before incision and continued postoperatively. In major open abdominal and thoracic
procedures, thoracic epidural blockade with local anesthetic can be a
rec-ommended anesthetic component of a postoperative ERP, providing excellent
analgesia, facilitating mobili-zation and physical therapy, and decreasing the
inci-dence and severity of ileus. However, the advantages of neuraxial blockade
are not as evident when mini-mally invasive surgical techniques are used.
Lumbar epidural anesthesia/analgesia should be discouraged for abdominal
surgery because it often does not pro-vide adequate segmental analgesia for an
abdominal incision. In addition, it frequently causes urinary
retention and lower limb sensory and motor
block-ade, increasing the need for urinary drainage cathe-ters (with
accompanying increased risk of urinary tract infection), delaying mobilization
and recovery, and increasing the risk of falls.
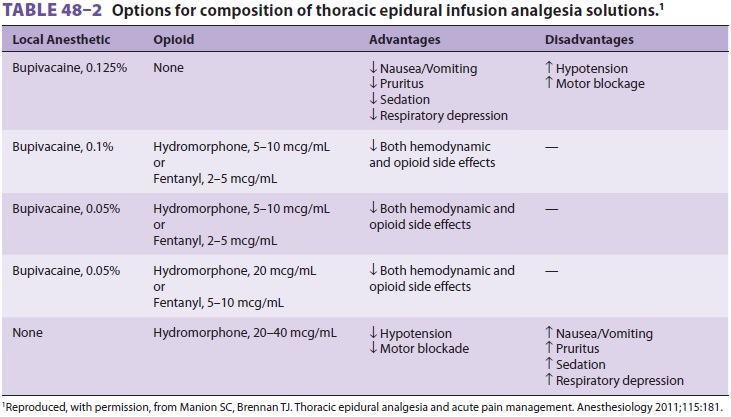
Epidural blockade using a solution of local
anes-thetic and low-dose opioid provides better postopera-tive analgesia at
rest and with movement thansystemic opioids (Figure 48–4 and Table 48–2). By sparing opioid use
and minimizing the incidence of systemic opioid-related side effects, epidural
analgesia facilitates earlier mobilization and earlier resumption of oral
nutrition, expediting exercise activity and attenuating loss of body mass.
Neural blockade minimizes postoperative insulin resistance, attenuating the
postoperative hyperglycemic response and facilitating utilization of exogenous
glucose, thereby preventing postoperative loss of amino acids and conserving
lean body mass.
If spinal anesthesia is used for fast-track
(and especially ambulatory) surgery, attention must be paid to delayed recovery
due to prolonged motor blockade. The use of smaller doses of intrathecal local
anesthetics (lidocaine, 30–40 mg; bupivacaine, 3–7 mg; or ropivacaine, 5–10 mg)
with lipophilic intrathecal opioids (fentanyl, 10–25 mcg, or sufent-anil, 5–10
mcg) can prolong postoperative analgesia and minimize the motor block without
delaying recovery from anesthesia. The introduction of ultra-short-acting
intrathecal agents such as 2-chloropro-caine (still controversial at present)
may further speed the fast-track process. Spinal opioids are asso-ciated with
side effects such as nausea, pruritus, and postoperative urinary retention.
Adjuvants such as clonidine are effective alternatives to intrathecal opi-oids,
with the goal of avoiding untoward side effects that may delay hospital
discharge. For example, intrathecal clonidine added to spinal local anesthetic
provides effective analgesia with less
urinary reten-tion than intrathecal morphine. Further studies are needed to
define the safety and efficacy of regional anesthesia techniques in fast-track
cardiac surgery (and many clinicians avoid them due to concerns about neuraxial
hematomas). Although some stud-ies have shown that spinal analgesia with
intrathecal morphine decreases extubation time, decreases length of stay in the
intensive care unit, reduces pul-monary complications and arrhythmias, and
pro-vides analgesia with less respiratory depression, other studies have shown no
benefit to this approach.
Continuous peripheral nerve blocks (CPNBs)
with local anesthetics block afferent nociceptive pathways and are an excellent
way to reduce the incidence of opioid-related side effects and facilitate
recovery . The choice of local anes-thetic, dosage, and concentration should be
made with the goal of avoiding prolonged motor blockade and delayed
mobilization and discharge. Ropiva-caine, because of its lower toxicity
relative to bupiva-caine, is often preferred when high volumes of local
anesthetic solution are needed. CPNB after knee arthroplasty facilitates
earlier discharge and rehabil-itation. Efforts must be made to minimize the
motor block of the quadriceps, which can be responsible for accidental falls.
Administering a lumbar plexus block along with a sciatic nerve block decreases
hospital length of stay, postoperative urinary reten-tion, and ileus associated
with lower extremity total joint replacement when compared with general or
neuraxial anesthesia followed by intravenous opi-oids. The same benefits of
fewer opioid side effects and accelerated discharge have been shown with regional
anesthesia/analgesia for hand, shoulder, anorectal, and inguinal
hernia repair surgery.
Advances in imaging techniques and
periph-eral catheter technology have generated interest in abdominal wall
blockade, facilitating the selective localization of nerves and the direct
deposition of local anesthetic in proximity to the compartments where the
nerves are located. Transversus abdominis plane (TAP) block has been used for abdominal surgery to
facilitate postoperative analgesia and early return of bowel function. Rectus
abdominis block can be used for midline incisions. These techniques are
alternatives to epidural block-ade when the latter is contraindicated.
The potential role of wound infusion of local
anesthetic solution in providing analgesia for ERAS has not been determined; nevertheless, local
anes-thetic wound infusions are widely used to improve postoperative pain
control and reduce the necessity for opioids.
C. Intravenous Lidocaine Infusion
Lidocaine (intravenous bolus of 100 mg or
1.5–2 mg/kg, followed by continuous intravenous infusion of 1.5–3 mg/kg/h or
2–3 mg/h) has analgesic, antihyperalgesic, and antiinflammatory properties. In
patients undergoing colorectal and radical retropubic prostate surgeries,
intravenous lidocaine has been shown to reduce requirements for opioids and
general anesthetic agents, to provide satisfactory analgesia, to facilitate
early return of bowel function, and to accelerate hospital discharge. Although
lidocaine infusion potentially may replace neuraxial blockade and regional
anesthesia in some circumstances, more studies are needed to confirm the
advantage of this technique in the context of ERPs. The most effective dose and
duration of infu-sion for various surgical procedures remains to be determined;
even short duration of lidocaine infu-sion may have benefit.
D. β-Blockade Therapy
Blockers have been used to blunt the
sympathetic response during laryngoscopy and intubation and to attenuate the
surgical stress-induced increase in cir-culating catecholamines. They also have
been shown to prevent perioperative cardiovascular events in at-risk patients
undergoing noncardiac surgery and to help maintain hemodynamic stability during
the intraoperative period and during emergence from anesthesia. β Blockers reduce the requirement of volatile
anesthetic agents and decrease minimum alveolar concentration values; they may
also have an opioid-sparing effect. They possess anticatabolic properties,
which may be explained by reduced energy requirements associated with decreased
adrenergic stimulation. A positive protein balance has been reported in
critically ill patients whenblockade is combined with parenteral nutrition. In
the context of ERPs, the anesthetic- and analgesic-sparing effects of β
blockers may facilitate recovery by accelerating emergence from anesthesia and
by reducing anesthetic- and analgesic-related postop-erative side effects,
including PONV.
E. Intravenous α2-Agonist Therapy
Both clonidine and dexmedetomidine have
anes-thetic and analgesic properties. Clonidine decreases postoperative pain,
reduces opioid consumption and opioid-related side effects, and prolongs
neur-axial and peripheral nerve local anesthetic blockade. In patients
undergoing cardiovascular fast-track surgery, spinal morphine with clonidine
decreases extubation time, provides effective analgesia, and improves quality
of recovery. Dexmedetomidine has not been extensively studied in ERP pathways.
Use of Short-Acting Intravenous & Inhalation Agents
A. Intravenous Anesthetics
Intravenous propofol is the deep sedation and
general anesthesia induction agent of choice for many surgi-cal procedures, and
may reduce the risk of PONV.
B. Inhalational Anesthetics
Compared with other volatile anesthetic
agents, desflurane and sevoflurane can shorten anesthesia emergence, reduce
length of stay in the postanesthe-sia care unit, and decrease
recovery-associated costs. When compared with propofol, all inhalation agents
increase the risk of PONV. Nitrous oxide, because of its anesthetic- and
analgesic-sparing effects, rapid pharmacokinetic profile, and low cost, is
frequently administered with other inhalation agents. However, its use may
increase the risk of PONV, and nitrous oxide is frequently avoided in patients
with risk fac-tors for PONV. Moreover, the use of nitrous oxide during
laparoscopic surgery may distend the bowel and impair the surgeon’s view of
anatomic structures .
C. Opioids
Short-acting opioids such as fentanyl, alfentanil, and remifentanil are
commonly used during fast-track surgery in combination with inhalation agents
or propofol, and with regional analgesia techniques. However, intraoperative
administration of remi-fentanil to patients who will experience extensive
postoperative pain has been associated with opioid-induced hyperalgesia, acute opioid
tolerance, and increased analgesic requirements during the post-operative
period.
D. Muscle Relaxants
The short-acting muscle relaxant
succinylcholine and intermediate-acting muscle relaxants such as rocuronium,
atracurium, and cisatracurium are commonly used to minimize the risk of
unplanned and prolonged muscle relaxation. They are chosen to facilitate
tracheal extubation while decreasing the risk of residual blockade during
anesthesia recovery.
Maintenance of Normothermia
The inhibitory effect of anesthetic agents on ther-moregulation,
exposure to the relatively cool sur-gical environment, and intraoperative loss
of heat through the surgical field can lead to intraoperative hypothermia in
all patients undergoing surgical procedures under general or regional
anesthesia. The duration and extent of the surgical procedure directly
correlate with hypothermia risk. Periop-erative hypothermia, by increasing
sympathetic discharge and inhibiting immune cellular response, increases
cardiovascular morbidity and wound infection risk. A decrease in core body
tempera-ture of 1.9°C triples the incidence of surgical wound infection. The
risk of bleeding and blood transfusion requirement are also increased with
hypothermia. Furthermore, by impairing the metabolism of many anesthetic
agents, hypothermia significantly pro-longs anesthesia recovery.
Maintenance of Adequate Tissue Oxygenation
Surgical stress leads to impaired pulmonary
function and peripheral vasoconstriction, resulting in arterial and local
tissue hypoxemia. Perioperative hypoxia can increase cardiovascular and
cerebral complica-tions, and many strategies should be adopted during the
perioperative period to prevent its development.
Maintenance of adequate perioperative
oxygen-ation by oxygen supplementation has been associated with the improvement
of some clinically relevant out-comes without increasing the risk of
postoperative complications. Ensuring complete recovery of neu-romuscular
blockade can reduce early postoperative hypoxemia. Intraoperative and
postoperative (for 2 h) inspired oxygen concentration of 80% has been
associated with increased arterial and subcutaneous oxygen tension, decreased
rate of wound infection, and lower incidence of PONV, but without increas-ing
potential complications associated with high oxygen fraction, such as
atelectasis and hypercapnia. However, these advantages have not been confirmed
in a large, randomized, multicenter trial of patients undergoing elective and
emergent laparotomy. The use of regional anesthesia techniques, by decreas-ing
systemic vascular resistance, can also improve superficial and deep peripheral
tissue perfusion and oxygenation. Finally avoidance of bedrest, and encouraging
early mobilization and physiotherapy, can also improve postoperative central
and periph-eral tissue oxygenation.
PONV Prophylaxis
Postoperative nausea and vomiting (PONV) is a
fre-quent complication associated with anesthetic drugs that delay early
feeding and recovery from surgery. Perioperative strategies for minimizing PONV
are strongly advocated for any type of surgery, and con-sensus guidelines for
prevention and management of PONV are available in the current literature.
Goal-Directed Fluid & Hemodynamic Therapy
Intraoperative and postoperative fluids are
com-monly infused in excess of perioperative loss. Despite numerous studies
seeking to define fluid strategy (amount and type of fluid administered,
crystalloid versus colloid, etc), “liberal,” “standard,” or “restrictive” fluid
regimens have failed to con-sistently improve postoperative outcomes. Liberal
fluid administration and sodium excess lead to fluid overload, increase
postoperative morbidity, and prolong hospitalization. Fluid overload,
espe-cially of crystalloid, has been associated with anas-tomotic leakage, pulmonary
edema, pneumonia, wound infection, postoperative ileus, and reduced tissue
oxygenation. Furthermore, excess fluids com-monly increase body weight by 3–6
kg and may impair postoperative mobilization. On the other hand, restrictive
fluid management does not offer any substantial, clinically relevant advantage,
except possibly improving pulmonary function and reduc-ing postoperative
hypoxia. However, compared with liberal fluid management, restrictive fluid
manage-ment increases the release of stress-related hor-mones such as
aldosterone, renin, and angiotensin
The amount of perioperative extracellular
fluid losses can be minimized with limited preoperative fasting, avoidance of
mechanical bowel preparation, minimally invasive surgical techniques such as
lapa-roscopic and video-assisted thoracoscopic (VAT) surgery, and early
postoperative enteral nutrition.
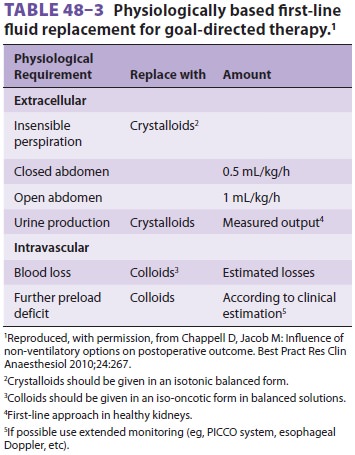
The concept of goal-directed fluid therapy is based on the optimization
of hemodynamic mea-sures such as heart rate, blood pressure, stroke vol-ume,
pulse pressure variation, and stroke volume variation obtained by noninvasive
cardiac output devices such as pulse-contour arterial waveform analysis,
transesophageal echocardiography, or esophageal Doppler. The type of fluid
infused is also important: isotonic crystal-loid should be used to replace
extracellular losses, whereas iso-oncotic colloids are needed to replace
intravascular volume ( Table 48–3).
Related Topics