Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Perioperative Pain Management & Enhanced Outcomes
Anesthetic Management: Issues in the Implementation of Enhanced Recovery Programs
Issues in the Implementation of Enhanced Recovery Programs
The success of ERPs depends upon the capacity
of multiple stakeholders to reach interdisciplinary con-sensus. Several aspects
of perioperative care, such as use of drains, dietary and activity
restrictions, fluid management, and bedrest, have been part of surgi-cal
“traditions” and must be significantly revised in ERPs. Patient involvement and
patient and family expectations are critically important, but frequently
overlooked, aspects of these programs. New surgical techniques, like transverse
incisions or minimally invasive surgery, may require surgeons to acquire and
perfect new skills. Similarly, the emphasis on thoracic epidural blockade or
peripheral nerve blocks, pharmacological modulation of the neuro-endocrine
stress response to surgery, goal-directed fluid and hemodynamic therapy, and
integral involvement of a well-organized and managed APS requires an expansion
of the traditional role of anes-thesia providers. Aggressive analgesia and
symptom management, early ambulation and physiotherapy, early nutrition
protocols, and early removal or total avoidance of urinary drainage catheters significantly
change the way patients are cared for in the post-anesthesia recovery unit and
on the surgical unit and require a well-organized, highly trained, highly
motivated nursing staff.
Although there are published studies of
suc-cessful ERPs, there are no “off-the-shelf” protocols,
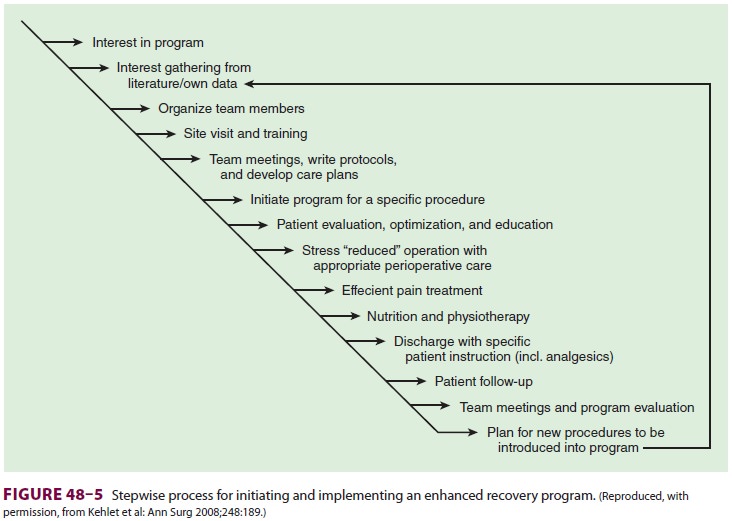
and local differences in expertise,
experience, and resources influence the development of such pro-tocols for each
institution. Each family of similar surgical procedures requires a standardized
interdis-ciplinary clinical protocol or pathway, with special-ized input from a
team with experience in caring for those patients. Such an interdisciplinary
team should include representatives from surgery, anesthesiol-ogy, nursing,
pharmacy, physiotherapy, nutrition, and administration, and it should be
responsible not only for the clinical protocol’s creation, but also for
continuously monitoring its efficacy and for insti-tuting performance
improvement-related protocol modifications and provider feedback as indicated
by outcomes data (Figure 48–5).
The current era is one in which optimal sur-gical care requires the
anesthesia provider to be part of the perioperative medicine team. The
anes-thesiologist’s skill sets are essential for the success of ERPs and have
potential benefits for surgical care delivery on a global basis, from
preoperative evaluation and presurgical preparation to recovery and final
dismissal from care. This opportunity must be seized
Related Topics