Chapter: Medical Surgical Nursing: Terrorism, Mass Casualty, and Disaster Nursing
Emergency Preparedness
EMERGENCY PREPAREDNESS
Federal, State, and Local Responses
There are many resources
available at the federal, state and local levels to assist in the management of
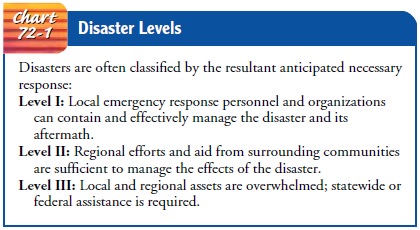
disasters and emergencies. Disasters are often assigned levels, which indicate
the anticipatedlevel of response (Chart 72-1). A list of the local resources
with specific instructions about how and when to contact them should be readily
available and frequently reviewed for needed updates. The following are a few
of the resources that may be of assistance during a mass casualty incident (MCI) or a disaster.
FEDERAL AGENCIES
There are many federal
resources that can be accessed through a process of requests. The state
authorities must request the feder-alization of resources through the proper
channels. This request for federal resources generally is made when local
resources have become or are in the process of becoming depleted.
Federal resources
include organizations such as Department of Health and Human Services (DHHS)
and the Department of Justice (DOJ). Each of these federal departments oversees
hundreds of agencies that may respond to MCIs. For example, the Federal Bureau
of Investigations (FBI) (under the DOJ) may be used for scene control and
collection of forensic evidence. The Federal Emergency Management Agency (FEMA)
can acti-vate teams such as the Urban Search and Rescue Teams (USRTs). The DHSS
administers the Centers for Disease Control and Prevention (CDC) and the
National Disaster Medical System (NDMS). The NDMS has many medical support
teams, such as Disaster Medical Assistance Teams (DMATs), Disaster Mortu-ary
Response Teams (DMORTs), Veterinary Medical Assistance Teams (VMATs), and
National Medical Response Teams for Weapons of Mass Destruction (NMRTs).
The DMAT provides medical personnel who can set up and
staff a field hospital; there are many DMATs located across the country. There
are only four NMRTs: the mobile California, North Carolina, and Colorado teams
and the Washington, DC team, which is stationary. These specialty teams were
developed to respond to situations involving WMDs. They consist of spe-cially
trained medical and technical personnel. The National Guard is also a resource,
with some guard units functioning as Civil Strike Teams (CSTs).
Also included in federal resources are the teams from the
CDC. This is the lead federal agency for disease prevention and control
activities and provides backup support to state and local health departments.
An additional support is available from the American Red Cross, which provides
many support systems and shelter as needed.
STATE AND LOCAL AGENCIES
Some of the state and local agencies may be the same agencies already listed (eg, local CDC and FBI agencies). Other state and local resources may include the American Red Cross, poison control centers, and other local volunteer organizations.
The Metro Medical Response Teams Systems (MMRS) are local teams that are
located in cities deemed to be possible terrorist targets and are funded for
specialty response to WMDs. Many state and federal task forces have been
developed to assist in the development and improvement of civilian medical
response to chemical and bio-logical terrorism.
Most cities and all
states have an Office of Emergency Man-agement (OEM). The OEM coordinates the
disaster relief efforts at the state and local levels. The OEM is responsible
for providing interagency coordination during an emergency. It maintains a
corps of emergency management personnel, including respon-ders, planners, and
administrative and support staff.
THE INCIDENT COMMAND SYSTEM
The Incident Command
System (ICS) is a management tool for organizing personnel, facilities,
equipment, and communication for any emergency situation. The federal
government mandates that the ICS be used during emergencies. Under this
structure, one person is designated as incident commander. This person must be
continuously informed of all activities and informed about any deviation from
the established plan (Currance & Bronstein, 1999; Lewis & Aghababian,
1996; Londorf, 1995). Whereas the ICS is primarily a field structure and process,
aspects of it are used at the level of an individual hospital’s emergency
response plan as well.
Hospital Emergency Preparedness Plans
Every facility is required by the Joint Commission on
Accredita-tion of Healthcare Organizations ( JCAHO) to create a plan for
emergency preparedness and to practice this plan twice a year (Burgess, Kirk,
Burron, & Cisek, 1999; JCAHO, 2000). Gener-ally these plans are developed
under the Environment of Care Committee or Safety Committee and are overseen by
an admin-istrative liaison.
Before the basic
emergency operations plan (EOP) can be de-veloped, the planning committee of
the facility first evaluates the community to anticipate the types of natural
and manmade dis-asters that might occur. This is not a difficult task and should
be a responsibility of the local facility, safety committee, safety of-ficer,
or emergency department (ED) manager. This information can be gathered by
questioning local law enforcement and fire de-partments and assessing the
amount of air or train traffic, auto-mobile traffic, and flood, earthquake,
tornado, or hurricane activity. Consideration is given to special situations
such as proximity to chemical plants, nuclear facilities, or military bases
that may en-hance the community’s potential for manmade disasters. Federal,
judicial, or financial buildings, schools, and any places where large groups of
people gather can be considered high-risk areas.The planning committee must
have a realistic understanding of its resources. It must determine, for example,
whether the fa-cility has a pharmaceutical stockpile available to treat
specific chemical or biological agents (Anteau, 1997; Stopford, 2000). Another
scenario that might be anticipated, the dispersal of a pul-monary intoxicant or
choking agent, requires that emergency op-erations planners find out how many
ventilators would be available in the facility and in the community. The
committee might also outline how staff would triage and assign priority to
patients when the number of ventilators is limited. Multiple fac-tors influence
a facility’s ability to respond effectively to a sudden influx of injured
patients, and the committee must anticipate var-ious scenarios to improve its
preparedness.
COMPONENTS OF EMERGENCY OPERATIONS PLAN
Once the initial assessment is complete, the facility
develops the
EOP. Essential components of the plan are as follows:
·
An
activation response: The EOP activation response of
ahealth care facility should define where, how, and when the response is
initiated.
·
An
internal/external communication plan: Communicationis critical
for all parties involved, including communication to and from the prehospital
arena (Heightman, 1999; Lewis & Aghababian, 1996; Mickelson, Burno, &
Schario, 1999).
·
A
plan for coordinated patient care: A response is planned
forcoordinated patient care into and out of the facility, in-cluding transfers
to other facilities. The site of the disaster can determine where the greater
number of patients may self-refer.
·
Security
plans: A coordinated security plan involving facilityand
community agencies is key to the control of an other-wise chaotic situation.
·
Identification
of external resources: External resources
areidentified, including local, state, and federal resources and information
about how to activate these resources.
·
A
plan for people management and traffic flow: “People man-agement”
includes strategies to manage the patients, the public, the media, and
personnel. Specific areas are assigned, and a designated person is delegated to
manage each of these areas (Anteau, 1997; Lewis & Aghababian, 1996).
·
A
data management strategy: A data management plan
forevery aspect of the disaster will save time at every step. A backup system
for charting, tracking, and staffing is devel-oped if the facility has a computer
system.
·
Deactivation
response: Deactivation of the response is as im-portant as
activation; resources should not be overused. The person who decides when the
facility is able to go from the disaster response back to daily activities is
clearly identified. Any possible residual effects of a disaster must be
considered before this decision is made (Anteau, 1997).
·
A
post-incident response: Often facilities see increased
volumesof patients up to 3 months after an incident. Post-incident response
must include a critique and a debriefing for all parties involved, immediately
and again at a later date.
·
A
plan for practice drills: Practice drills that include
com-munity participation allow for troubleshooting any issues before a
real-life incident occurs.
·
Anticipated
resources: Food and water must be available forstaff, families, and
others who may be at the facility for an extended period.
·
Mass
casualty incident planning: MCI planning includessuch
issues as mass fatality and morgue readiness.
·
An
educational plan for all of the above: A strong educationalplan
for all personnel regarding each step of the plan allows for improved readiness
and additional input for fine-tuning of the EOP (Howard, 2001; Kotzmann, 1999;
Anteau, 1997; Burgess et al., 1999; Lewis & Aghababian, 1996; Heightman,
2000; Levitin & Siegelson, 1996).
The EOP should also
include a structure that defines roles for all employees in each emergency
situation. The most common structure is the ICS described earlier, but applied
at the level of the hospital itself instead of at the site of the disaster. For
exam-ple, an administrator, possibly the nurse executive, will act as In-cident
Commander within the hospital and coordinate all aspects of the implementation
of the plan. Other personnel will be des-ignated to perform key roles, such as
resource manager or patient disposition coordinator. Such a predetermined
organization is es-sential to minimize confusion, ensure that all key
operations are directed, and promote a well-coordinated response.
Related Topics