Chapter: Essential Anesthesia From Science to Practice : Clinical management : General anesthesia
Early post-operative care - Anesthesia
Post-operative care
The
post-operative care of the patient can be divided into an early and a continued
phase. The early phase lasts from the moment the patient leaves the operating
room until he is discharged from the Post-Anesthesia Care Unit (PACU) or its
equi-valent. The care is then continued, a phase that can extend for days or even
weeks.
Early post-operative care
Based on
his medical condition and the planned operative procedure, we will have
classified the patient as ambulatory (also known as outpatient), as
‘post-operative admit’ (the patient comes to the hospital on the day of the
operation and is admitted to the hospital after his operation), or as an
inpatient (the patient is already in the hospital, or will be admitted for
pre-operative preparation, and will stay there post-operatively). Two
categories of patients might bypass the PACU (formerly called the Recovery
Room): (i) ambulatory patients who had a minor procedure and are expected to be
ready for discharge in a matter of minutes and (ii) patients requiring
intensive care because of serious pre-operative med-ical problems or major
operations with potential complications. Such patients are admitted directly to
the Intensive Care Unit (ICU) upon completion of the operation.
For patients coming to the PACU we consider
three factors: the patient’s pre-operative condition; the effects of the just
completed therapeutic (surgical, radio-logical, obstetrical, electroconvulsive)
or diagnostic procedure; and the effects of the anesthetic. As we turn the
patient’s care over to the PACU staff, we provide a formal “report” of his condition
including the following:
·
pre-existing medical conditions with particular emphasis on
pre-existing respiratory, cardiac, and chronic pain issues;
·
surgical disease, operative and anesthetic course, and any problems
encoun-tered;
·
fluid status including what was administered, estimated blood loss,
and urine output;
·
medications administered in the operating room. We mention
antagonists given to counteract lingering neuromuscular weakness or respiratory
depression or nausea and vomiting. Should the patient need more such
medication, the PACU physician can either continue the already initiated
treatment or, if the patient does not respond, switch to another drug;
·
concerns regarding the procedure or the patient, including the plan
for post-operative pain management;
·
issues requiring follow-up such as pending laboratory evaluations
or a chest radiograph to confirm central venous catheter placement.
Finally,
we make certain the patient is stable, record a first set of vital signs
obtained in the PACU, and ensure that all documentation is complete and
correct.
In the
PACU, we first worry about safety. We consider waning anesthetic drug effects
as they relate to adequacy of oxygenation, which in turn requires an alert
respiratory center (is there a hangover effect from CNS depressants?) and the
muscle power to breathe (is there a hangover effect from muscle relaxants or a
regional anesthetic?), an open airway (is there obstruction of the upper
airway?), and no encumbrance to breathing from dressing, position, or the
surgical proce-dure. Adequacy of oxygenation also requires adequate circulation
(is the blood pressure normal and the ECG unchanged from its preoperative
state?). The pulse oximeter will speak volumes to these questions. If the
patient is breathing roomair and his
oxygenation (as measured by pulse oximetry located peripherally) isnormal, we
can be assured of adequate breathing.
We
assess the central nervous system, recognizing that the patient usually will
have had a number of drugs with CNS effects. With modern anesthetic techniques
and drugs, we expect the patient to rally from the depressant effects of the
drugs fairly rapidly and to become responsive, if not immediately oriented. Up
to 25% of elderly patients will be delirious after a general anesthetic for a
major surgical procedure. Once a patient is not only responsive but also
oriented, we know that his brain is perfused and oxygenated.
Most
patients will arrive with an intravenous infusion. If we assume that the
patient is in a neutral fluid balance (blood pressure and urine output back to
preoperative values), in short, if his insensible losses (about 800 mL/day) and
intra-operative losses (from evaporation from exposed surfaces, e.g.,
intestines, bleeding and from edema caused by the surgical trauma (the
so-called third space or blister)) have been replaced, fluid therapy will
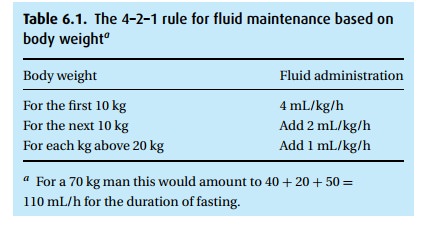
simply continue to replace insen-sible losses following the 4–2–1 rule (see
Table 6.1).
Often
enough, however, some bleeding continues – usually invisibly – into the traumatized
tissue. Fluid therapy will need to be adjusted to meet the patient’s
requirements as judged by cardiovascular signs and urine production. A
bal-anced salt solution such as normal saline or Ringer’s lactate will serve as
long as there is no need to worry about electrolytes, red blood cells, and
plasma proteins.
Early post-operative pain
As we
reassure ourselves as to the patient’s safety, we begin to consider the
patient’s pain. Three points need attention: (i) surgical incisional pain will
decrease over time, (ii) analgesic effects left over from the anesthetic will
wane over time, and (iii) pain counteracts the CNS depressant (respiratory)
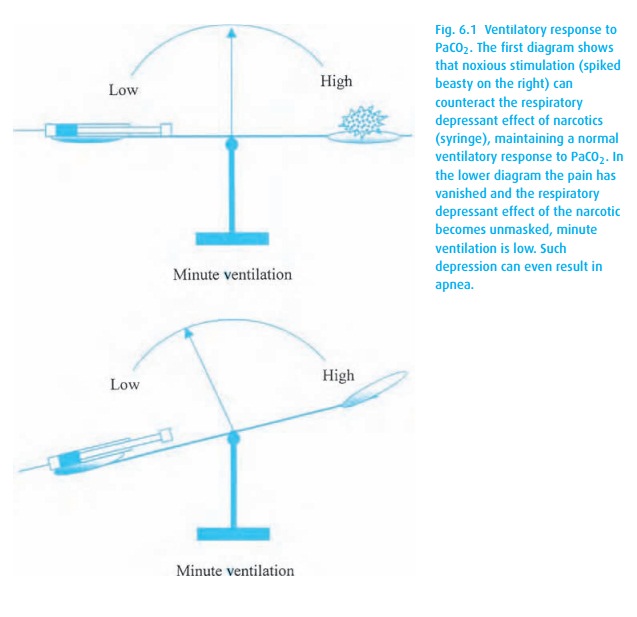
effects of narcotic analgesics (Fig. 6.1).
Thus, pain management in the PACU must seek a balance of three shifting slopes
of which we do not know the rate of change. This translates into: watch the patient and titrate drugs to
balance adequate analgesia and avoid respir-atory depression. As long as the
patient cannot take oral medication, a practical approach for the acute phase
of pain management in the PACU can make use of intravenous morphine in 2.0 mg
increments for the average adult. It takes about 5 minutes for such a dose to
show an effect. Therefore, wait at least 5 minutes before giving the next dose.
Many factors influence the patient’s response to such treatment. A patient on
chronic narcotic therapy will require more, a frail elderly person less.
Titrate! Titrate! Titrate!
After
minor surgical procedures, many patients will not require opioids at all, and
most can take oral medication. The pharmacology chapter gives drugs and
dosages.
There
would be no need for a PACU if it were not for the occasional complica-tions
that require early recognition and prompt treatment. Here is a quick review of
potential problems encountered in the PACU.
Complications
Desaturation
Differential diagnosis
·
Hypoventilation Always first assist ventilation
to establish normal SpO2 and PaCO2! Then consider causes and their treatment.
Residual neuromuscular blockadeSuspected when the patient shows anabnormal
respiratory pattern, particularly the tracheal tug, i.e., downward motion of
the larynx with inspiration. Test with the twitch monitor. Treat with reversal
agents.
– Residual sedationConsider reversal of benzodiazepines with
flumazenil.
– NarcosisTypically a slow, deep respiratory pattern;
consider cautious reversalof opioids with naloxone.
– Bronchospasm (wheezing)Intubation is a strong stimulant for
bronchospasm;treat with bronchodilators.
– Laryngospasm (stridor)If related to the operation, e.g., neck
operation withpossible hematoma formation, it becomes a surgical emergency. Try
continu-ous positive airway pressure, letting the patient exhale against
resistance (5 to 10 cmH2O) and maintaining that pressure throughout
the respiratory cycle.
– PainParticularly with a subcostal incision where
deep breathing is painful.
·
Ventilation/Perfusion mismatch
– AtelectasisProbably the most common cause of
post-operative hypoxemia.
– Aspiration of gastric
contentsParticularly
in high-risk patients, or if intubationrequired multiple attempts.
– PneumothoraxEspecially after central venous access. Obtain
a chest radio-graph, but be prepared to relieve the pneumothorax by puncture
(2nd inter-costal space, mid-clavicular line) should a tension pneumothorax
develop in the meantime.
– Pulmonary embolismThromboembolism is the most common. May needV/Q
or CT scanning. Most surgical patients require some form of prophylaxis against
deep vein thrombosis (DVT).
– Pneumonia
– Mainstem intubation
·
Diffusion block
– Pulmonary edema
·
Inadequate FiO2
Management
(i)Airway
Chin
lift, neck extension; continuous positive airway pressure (CPAP) often helps.
For this, use a bag and mask system (Mapleson – see The anesthesia machine)
with a high flow (15 L/min) of oxygen. Apply the face mask tightly, letting the
patient exhale against resistance (5 to 10 cmH2O) and maintain that
pressure throughout the respiratory cycle.
(ii) Breathing
·
Supplemental oxygen
– Via nasal cannula, but with oxygen flows of 2 L/min the inspired O2only
increases by about 6%.
– Via
standard tent face mask for an inspired O2of up to 50%
– Via partial rebreathing face mask for an inspired O2of
up to 80%
– Via non-rebreathing face mask for an inspired O2of up to
95%
·
Encouragement – “take a breath!” often effective with narcotic
depression
·
Bag–Mask – use with self-inflating bag or Mapleson
·
Check ventilator settings, O2 supply and end-tidal CO2
if the patient is intubated.
(iii)
Studies to consider
·
Chest radiograph if abnormal breath sounds (pneumonia, atelectasis,
pneumothorax, +/− aspiration). Keep in mind, however, that a
portable film may not provide the highest quality and consolidation takes some
time to manifest radiographically.
·
Arterial blood gas
·
Twitch monitor if patient appears to be partially paralyzed.
Hypotension
Differential diagnosis
·
Inadequate preload
– Inadequate fluid resuscitation
– Continued hemorrhage
– Venodilation due to medications or sympathetic blockade
– Pericardial tamponade
– Pulmonary embolism
– Increased intra-abdominal pressure, e.g., big uterus pressing on
vena cava
– Increased intra-thoracic pressure, e.g., tension pneumothorax
·
Poor contractility
– Residual anesthetics
– Myocardial ischemia
– Fluid overload (“far-side” of the Starling Curve)
– Pre-existing cardiac dysfunction
– Electrolyte disturbance
– Hypothermia
·
Inadequate afterload
– Sepsis
– Vasodilation due to medications or sympathetic blockade, e.g.,
neuraxialanesthetic
– Anaphylaxis
·
Arrhythmias
– Bradycardia
– Loss of atrial kick
Atrial
fibrillation/flutter AV dissociation
– Electrolyte disturbance
Management
·
Physical examination (especially chest auscultation)
·
ECG (at least 5-lead strip) to detect arrhythmias and ischemia ACLS
protocol if abnormal rhythm
·
Hemoglobin level
·
Intravascular fluid resuscitation +/− blood transfusion Supplemental oxygen
·
Elevate legs to enhance venous return Consider transthoracic echo
·
Consider chest radiograph
·
Consider invasive monitoring
·
Check electrolytes, especially Ca2+ for inotropy and K+ , Mg2+ for arrhythmias
Hypertension
Differential diagnosis
·
Pain
·
Pre-existing hypertension Bladder distension
·
Rebound hypertension (especially with chronic clonidine) Endocrine
problem (thyroid storm, pheochromocytoma) Malignant hyperthermia
·
Delirium tremens
·
Increased intracranial pressure
Management
·
Treat pain or anxiety if present.
·
Review for pre-existing hypertension and reinstitute
anti-hypertensive therapy where appropriate.
·
Check ECG.
·
Look for additional signs of malignant hyperthermia.
·
Check for high bladder dome. If Foley catheter in place, check
patency, or per-form in-and-out catheterization.
We hope
that none of these problems arose or that they have been dealt with
successfully, at which point we are ready to discharge the patient from the
PACU.
PACU discharge
A
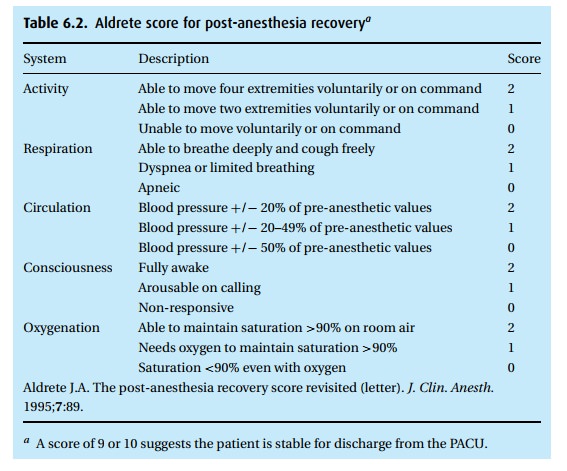
frequently used checklist is the Aldrete Recovery Score (see Table 6.2). If the sum of points reaches 9 or 10, we can
discharge the patient from the PACU.
Outpatients
After
outpatient procedures under local or peripheral nerve block anesthe-sia,
perhaps with parenterally administered CNS depressants, e.g., midazolam
(Versed®), propofol or opioids, the patient may bypass the PACU unless a
med-ical condition would call for observation. It may be necessary to prescribe
an oral analgesic that might include a mild opioid.
If no CNS depressant drug was used during the procedure and if the peripheral nerve block is behaving as expected (surgical anesthesia wearing off, but perhaps analgesia continuing), the patient can be discharged. We still insist that a relative or friend accompany them home because the patient will have been exposed to the stress of an operation – however minor – and will have been fasting and thus be at risk of swooning or even fainting and not being at the height of his reflex responses.
For
those patients who required CNS depressants for a short operative proce-dure in
which no severe post-operative pain is expected, e.g., a sigmoidoscopy under
propofol sedation or a cataract removal under local anesthesia preceded by a
small (0.5 to 0.75 mg/kg) dose of methohexital (Brevital®) to minimize the
discomfort of the retrobulbar block, the recovery process can be completed in a
matter of minutes to an hour, at which point the patient can be discharged into
the care of a relative or friend for transportation home. We always assume that
drug effects and hormonal disturbances will linger for a matter of several
hours to a day, so that upon discharge, the patient cannot be considered ready
to drive an automobile or ride a bicycle or even cross the street by himself.
For
those patients who remain in the hospital following their operation, PACU
discharge signals the phase of continued post-operative care.
Related Topics