Chapter: Essential Anesthesia From Science to Practice : Clinical management : General anesthesia
Continued post-operative care - Anesthesia
Continued post-operative care
The
patient will go through important changes in response to a major operation with
anesthesia. The stress of the inflicted surgical trauma will trigger a release
of adrenocorticotropic hormones, cortisol, and catecholamines. Catabolism will
overpower anabolism; the patient will be in a negative nitrogen balance.
Coagulation
changes might further thrombosis. Incisional pain and narcotic anal-gesics can
reduce pulmonary gas exchange. Narcotics inhibit the cough reflex, already
reduced in the elderly, causing patients to retain bronchial secretions, potentially
leading to atelectasis and pneumonitis. Large fluid loads given dur-ing the
operation need to be mobilized, yet antidiuretic hormone secretion will favor
water and salt retention. An ileus after intra-abdominal procedures often takes
days to resolve while nasogastric suction deflates the stomach not without
removing electrolytes. In short, many major operations will leave the patient
in a greatly debilitated state that can take several days to resolve.
If these
processes are superimposed on extensive surgical operations, for exam-ple those
affecting heart, lung or brain, the patient will be admitted to the ICU. This
will also be true for post-operative patients who come with pre-existing
disease processes involving the cardiovascular (congestive heart failure,
recent myocar-dial infarction), or respiratory (obstructive lung disease)
systems, the central ner-vous system (stroke, tumor), metabolism (diabetes),
hepatic or renal systems, or infection. The available frequency of observation,
extent of monitoring, and immediacy of care in the ICU does not match what is
available in the operating room, but greatly exceeds whatever can be offered on
the post-surgical ward.
When we
visit the patient on the post-surgical ward, we will not only consult his chart
to see the trends in vital signs (cardiovascular, respiratory and temperature)
but also assess fluid status and medications prescribed and given. We then talk
to the patient to gauge his mental status (up to 25% of elderly patients can
take up to a week to become fully oriented, and some 10% have cognitive
impairment lasting for months) and to ask about his comfort. We might have to
explain that hoarse-ness (from an endotracheal tube) or a sore throat (from an
LMA or endotracheal tube) are likely to improve in a day or two. We continue to
worry about pulmonary complications, e.g., atelectasis and pneumonitis, which
are most likely in elderly men, in smokers, and after operations that involve
the upper abdomen and the chest. Being aware that myocardial infarctions are
far more likely to occur – many of them silently – on the second post-operative
day than in the operating room, we pay special attention to the cardiovascular
system. Hypotension, hypertension (often pre-existing), and arrhythmias are not
uncommon.
Pain management
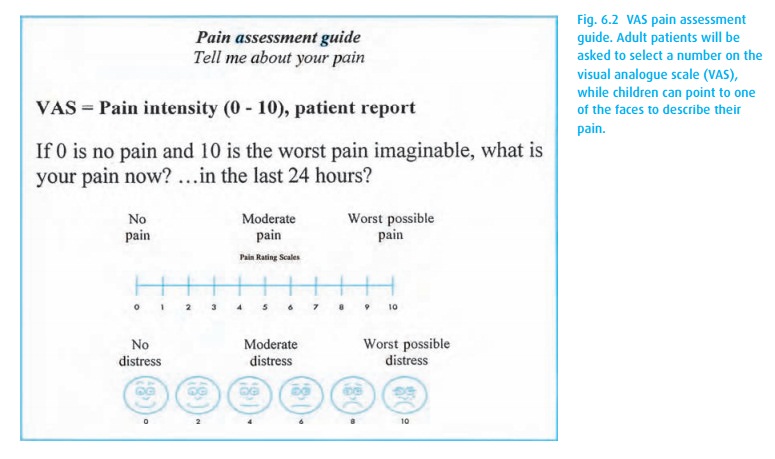
As
anesthesiologists, we are particularly attentive to the patient’s pain and its
management. We now use a widely employed standardized method of assessing pain
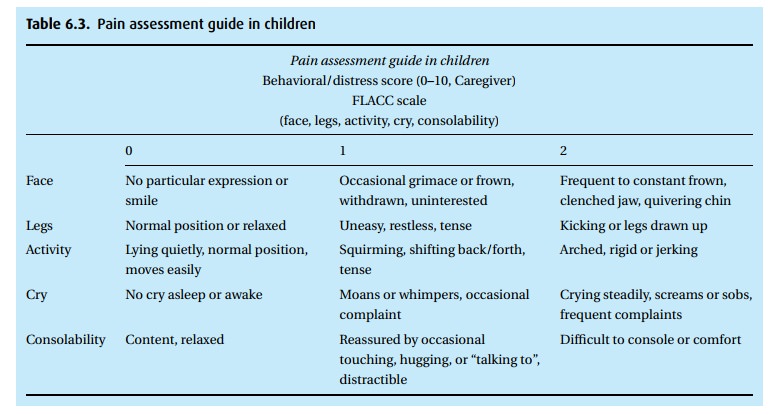
in adults and children (Fig. 6.2). In
children incapable of relating their pain, physical signs can help (Table 6.3). The treatment of pain will be influenced by
its severity.
If the patient is unable to take oral medication, we can institute patient-controlled intravenous opioid administration (PCA), a system that enables the patient to trigger an intravenous injection of a predetermined amount of a nar-cotic.
The PCA pumps can be programmed to deliver a specific volume, then to lock the
system for a predetermined period. When the patient pushes a button, a typical
program might deliver (into a running intravenous drip) a 1 mL bolus containing
1.0 mg morphine. The pump then goes into a lockout mode, making an additional
injection impossible for a preprogrammed period of, for example, 5 minutes. The
pump can be programmed to limit the hourly injection to, for example, no more
than 12 mg/h. Even that amount will be excessive if the patient were to
self-administer the maximum, hour after hour. The dose and the lock-out period
have to be tailored for the individual patient. While morphine is the
stan-dard, several drugs are available, among them hydromorphone (Dilaudid®)
and fentanyl. In addition, for patients who pre-operatively have become
tolerant to opioids, a background infusion of the narcotic may be required.
Depending
on the operation (some cause much more severe and protracted pain than others;
some limit oral intake for a longer period) and the patient (some are much more
sensitive than others), a PCA pump might be available to the patient for a day
or a week or more. Once narcotics are no longer needed, or the patient can
tolerate p.o. intake, oral medications take over. A great variety of drugs are
available (see Pharmacology).
Some
patients will still have an epidural catheter in place that had served the
anesthetic management during a thoracic, abdominal or lower extremity
oper-ation and can now be used for pain management. Typically, we infuse a low
concentration of local anesthetic combined with a narcotic through the
catheter. By combining these drugs, we minimize the amount of motor block
(paralysis) from the local anesthetic while limiting narcotic side effects
(nausea, itching, and urinary retention) associated with larger doses of
opioids. Once we establish a level of analgesia with a bolus injection, an
infusion is begun and the patient might regulate the administration of
additional drug with a PCA pump (PCEA: patient controlled epidural analgesia).
Dose and concentration of local anes-thetic and lock-out period will have to be
adjusted for the individual patient and drugs infused. A typical arrangement
might deliver 0.2 mg of morphine in 1.0 mL fluid containing 0.25% bupivacaine
and a lock-out period of 10 minutes. Other approaches use a continuous epidural
infusion alone.
The
post-operative recovery will progress slowly. Every day, if all is going well,
we can see improvements. Indeed, we can often see the moment when the patient
‘turns the corner’ from negative to positive nitrogen balance. He will start
shaving, she will do her hair and even put on lipstick. The patient will begin
to eat, and we can switch from parenteral to oral medication. Many patients
will be discharged from the hospital with prescriptions for oral analgesics.
See the Pharmacology chapter for a list of commonly used drugs, dosages and
duration of effect.
Related Topics