Chapter: Basic & Clinical Pharmacology : Antimycobacterial Drugs
Drugs Active Against Atypical Mycobacteria
DRUGS ACTIVE AGAINST ATYPICAL MYCOBACTERIA
About 10% of
mycobacterial infections seen in clinical practice in the United States are
caused by nontuberculous or “atypical” mycobacteria. These organisms have
distinctive laboratory charac-teristics, are present in the environment, and
are generally not communicable from person to person. As a rule, these
mycobacte-rial species are less susceptible than M tuberculosis to antitubercu-lous drugs. On the other hand, agents
such as erythromycin, sulfonamides, or tetracycline, which are not active
against tuberculosis, may be
effective for infections caused by atypicalmycobacteria. Emergence of
resistance during therapy is also a problem with these mycobacterial species,
and active infection should be treated with combinations of drugs. M kansasii is sus-ceptible to rifampin
and ethambutol, partially resistant to isoni-azid, and completely resistant to
pyrazinamide. A three-drug combination of isoniazid, rifampin, and ethambutol
is the con-ventional treatment for M
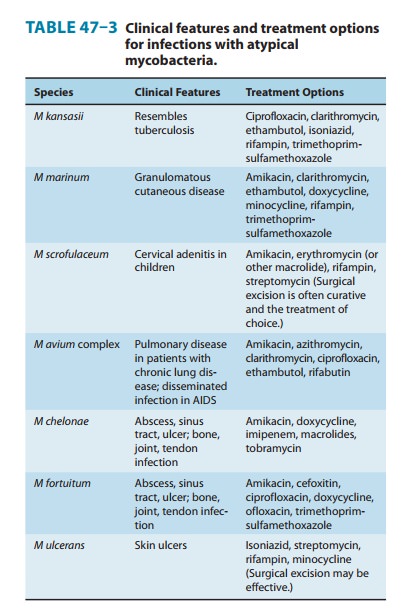
kansasii infection. A few representative pathogens, with the clinical
presentation and the drugs to which they are often susceptible, are given in
Table 47–3.
M avium complex (MAC), which includes both M avium and intracellulare, is an important and common cause of dissemi-nated disease in late stages of AIDS (CD4 counts < 50/μL). MAC is much less susceptible than M tuberculosis to most antitubercu-lous drugs. Combinations of agents are required to suppress the infection. Azithromycin, 500 mg once daily, or clarithromycin, 500 mg twice daily, plus ethambutol, 15–25 mg/kg/d, is an effective and well-tolerated regimen for treatment of disseminated disease. Some authorities recommend use of a third agent, such as ciprofloxacin, 750 mg twice daily, or rifabutin, 300 mg once daily. Other agents that may be useful are listed in Table 47–3. Azithromycin and clarithro-mycin are the drugs of choice for reducing the incidence of MAC bacteremia in AIDS patients with CD4 cell counts less than 100/μL.
Rifabutin in a single
daily dose of 300 mg has been shown to reduce the incidence of MAC bacteremia
but is less effective than macrolides.
Related Topics