Chapter: Modern Pharmacology with Clinical Applications: Therapy of Human Immunodeficiency Virus
Drug Therapy of HIV Infection: Protease Inhibitors
Protease Inhibitors
These drugs inhibit the
activity of HIV protease. This enzyme, which is required for the production of
a ma-ture infectious virus, cleaves the gag-pol polyprotein into structural
proteins and active enzymes. The phar-macokinetic parameters of the protease
inhibitors are listed in Table 51.5.

The protease inhibitors are
used in the multidrug therapy of HIV infection. Resistance to the HIV pro-tease
inhibitors results from mutations in the protease gene and perhaps the cleavage
sites of gag-pol. Although different protease mutations tend to be asso-ciated
with resistance to individual drugs, resistance to one protease inhibitor is
often associated with a less than optimal response to other agents of this
class. Indinavir, ritonavir, and lopinavir require more muta-tions to lose
their effectiveness than do the other pro-tease inhibitors.
All protease inhibitors can
produce nausea, vomit-ing, diarrhea, and paresthesia. Drug-induced
hyper-glycemia and insulin resistance may precipitate the onset of diabetes
mellitus or worsen existing cases. Protease inhibitors may also cause
hypercholester-olemia and hypertriglyceridemia. Liver enzymes may be increased,
and hepatic toxicity may occur at high doses. Fat redistribution is common and
can manifest as central fat accumulation, peripheral wasting, buffalo hump at
the base of the neck, breast enlargement, and/or lipomas.
Protease inhibitors may
increase the risk of bleeding in hemophiliacs. These drugs should be used with
cau-tion in patients with diabetes, lipid disorders, and he-patic disease.
Dosage adjustment may be necessary.
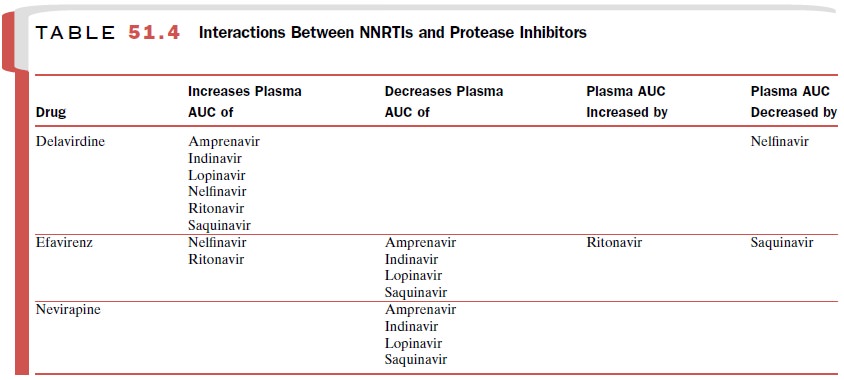
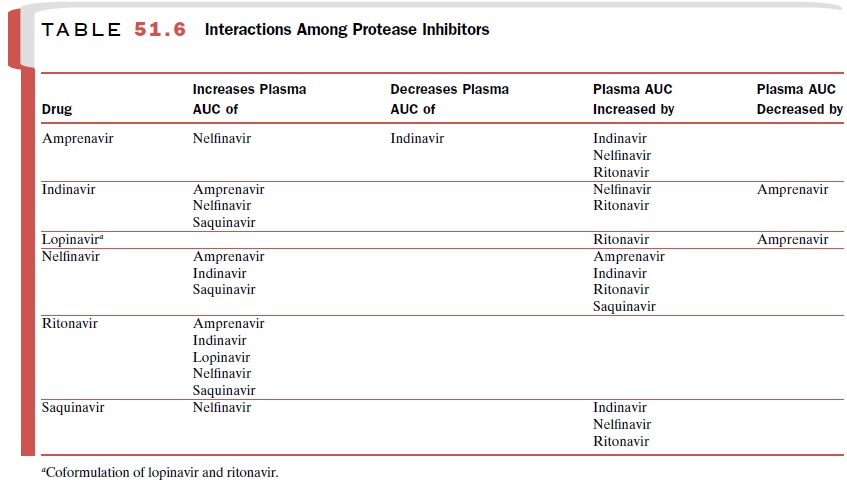
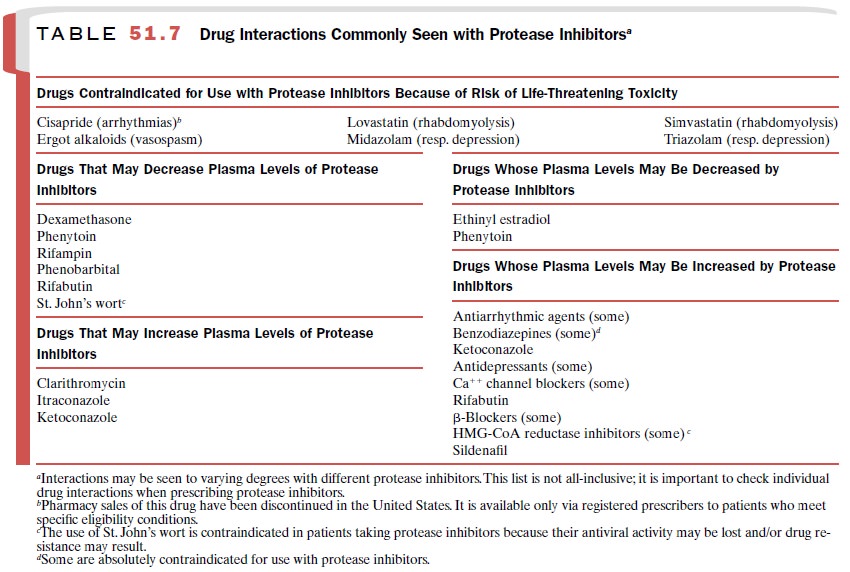
Protease inhibitors interact with a large number of drugs because
they are metabolized by and inhibit CYP3A4. Ritonavir is the most potent inhibitor of CYP3A4, with indinavir, amprenavir, and
nelfinavir be-ing much less potent and saquinavir the least potent. When given
as part of a combination therapy, the pro-tease inhibitors affect plasma levels
of NNRTIs as well as each other (Tables 51.4 and 51.6). Many drugs inter-act
with protease inhibitors by inhibiting or inducing their metabolism; similarly,
protease inhibitors inhibit or induce the metabolism of numerous drugs (Table
51.7).
Saquinavir
Saquinavir is a potent
inhibitor of HIV-1 and HIV-2 protease. Fortovase,
a soft gel preparation of saquinavir, has largely replaced saquinavir mesylate
capsules (Invirase) because it has
improved bioavailability. Saquinavir is usually well tolerated and most
frequently produces mild gastrointestinal side effects.
Ritonavir
Although ritonavir (Norvir) is a potent inhibitor of HIV-1
and HIV-2 protease, it is not well tolerated in higher doses. It is mainly used
in low doses to increase blood levels of other protease inhibitors and to
extend their dosing interval. Ritonavir is more commonly asso-ciated with
gastrointestinal side effects, altered taste sensation, paresthesias, and
hypertriglyceridemia than are other protease inhibitors. Pancreatitis may occur
in the presence or absence of hypertriglyceridemia.
Of all the protease inhibitors, ritonavir is the most po-tent
inhibitor of CYP3A4; therefore, it tends to produce more frequent and severe
interactions with other drugs. It inhibits an additional cytochrome P450
isozyme, CYP2D6, and can increase plasma concentrations of drugs that are
metabolized by it (e.g., most antidepres-sants, some antiarrhythmics, some
opioid analgesics, some neuroleptics). For example, ritonavir should not be
used in conjunction with amiodarone, bepridil, fle-cainide, propafenone,
quinidine, or pimozide. In addi-tion to CYP3A4, ritonavir induces CYP1A2 and
possi-bly CYP2C9 and may inhibit the breakdown of drugs metabolized by these
enzymes.
Indinavir
Indinavir (Crixivan) is a potent inhibitor of HIV
re-verse transcriptase. It produces the side effects common to all protease
inhibitors and also may produce nephrolithiasis, urolithiasis, and possibly
renal insuffi-ciency or renal failure. This
problem occurs more frequently in children (approximately 30%) than adults
(approximately 10%) and can be minimized by drinking at least 1.5 L of water
daily. Additional side effects in-clude asymptomatic hyperbilirubinemia,
alopecia, in-grown toenails, and paronychia. Hemolytic anemia rarely occurs.
Rifampin should not be given with indi-navir.
Nelfinavir
Nelfinavir (Viracept) is probably the most commonly
used protease inhibitor because of its low incidence of serious adverse
effects. Its most common side effects are diarrhea and flatulence; these may
resolve with con-tinued use. In addition to the drugs contraindicated for use
with all protease inhibitors, amiodarone, rifampin, and quinidine are
contraindicated in patients taking nelfinavir.
Amprenavir
Amprenavir (Agenerase) is administered twice daily,
providing the patient with an advantage over other pro-tease inhibitors that
must be taken more frequently (e.g., indinavir, saquinavir). Common side
effects of am- prenavir include nausea, vomiting, diarrhea, and perio-ral
paraesthesias. Rash occurs in approximately 20 to 30% of patients and can be
mild or severe (Stevens-Johnson syndrome).
Amprenavir oral solution contains large amounts of the excipient
propylene glycol and should not be given to children under age 4 because it can
produce hyperosmo-lality, lactic acidosis, seizures, and/or respiratory
depres-sion. Pregnant women should not take amprenavir oral solution, as fetal
toxicity may result. Amprenavir is a sul-fonamide and should be used with caution in
patients with sulfonamide allergy. Amprenavir oral solution and capsules
contain high levels of vitamin E; therefore, pa-tients are advised not to take
supplemental vitamin E. In addition to the drugs contraindicated for use with
all protease inhibitors, amprenavir should not be given with pimozide or
rifampin.
Lopinavir–Ritonavir
Lopinavir is available in the
United States only as a fixed-dose combination with ritonavir (Kaletra). In this regimen, a low dose
of ritonavir is used to inhibit the rapid inactivation of lopinavir by CYP3A4. Side
effects, which are generally mild,
include diarrhea, nausea, as-thenia, and headache. Pancreatitis occurs rarely.
Ritonavir is a potent inhibitor of CYP3A4 and also in-hibits CYP2D6. In
addition to the drugs contraindi-cated for all protease inhibitors, flecainide,
propa-fenone, pimozide, and rifampin should not be given with
lopinavir–ritonavir combination therapy.
Related Topics