Chapter: Modern Pharmacology with Clinical Applications: Insulin and Oral Drugs for Diabetes Mellitus
Diabetes Mellitus
DIABETES
MELLITUS
Diabetes mellitus affects
approximately 5 to 8% of the population. A large number of individuals are asympto-matic
and do not know they have the disease. The re-cent rise in obesity in the
United States accounts for much of the observed and anticipated rise in cases
of di-abetes mellitus in this country. Although insulin treat-ment has greatly
increased the life expectancy of the di-abetic patient, diabetes remains the
third leading cause of death by disease, the second leading cause of
blind-ness, and the second leading cause of renal failure.
Diabetes mellitus is a
heterogeneous group of disor-ders characterized by abnormalities in
carbohydrate, protein, and lipid metabolism. The central disturbance in
diabetes mellitus is an abnormality in insulin produc-tion or action or both,
although other factors can be in-volved. Hyperglycemia is a common end point for
all types of diabetes mellitus and is the parameter that is measured to
evaluate and manage the efficacy of dia-betes therapy.
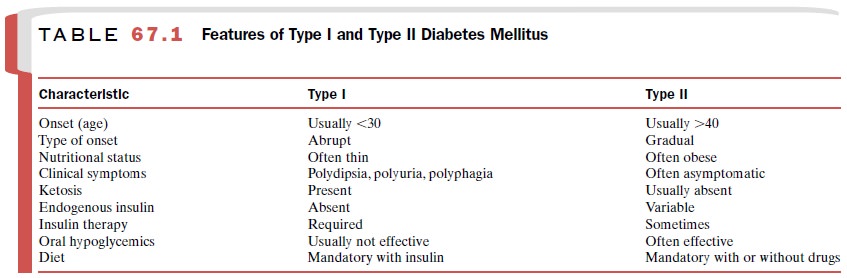
Diabetes mellitus has been
traditionally classified into insulin-dependent
diabetes mellitus (IDDM), also known as type I- (formerly called juvenile-onset
dia-betes mellitus), and non–insulin-dependent
diabetes mellitus (NIDDM), also known as type II (formerly re-ferred to as
adult-onset diabetes mellitus). There are clearly varying degrees of overlap,
and though it is often important to know whether a particular individual
pos-sesses relative insulin deficiency or relative insulin re-sistance or both,
some of the more salient differences between IDDM and NIDDM are summarized in
Table 67.1.
The pathogenesis of type I- diabetes is autoimmune destruction of
the cells of the pancreas. The factor or fac-tors that trigger this autoimmune response are
un-known. Predisposing factors appear to include certain major
histocompatibility complex haplotypes and au-toantibodies to various islet cell
antigens. The progres-sion of the autoimmune response is characterized by
lymphocytic infiltration and destruction of the pancre-atic cells resulting in
insulin deficiency. Type I- diabetes mellitus constitutes about 10% of cases of
diabetes mellitus.
The other type of diabetes
mellitus, type II, is far more common. In contrast, type II is not an
autoimmune process and may or may not be insulin dependent; that is, a diabetic
state that is most effectively managed by in-sulin therapy. Frequently, NIDDM
is used interchangeably with type II diabetes mellitus, and efforts are being
made to avoid the term adult onset, since many adoles-cents (and occasionally
children) are developing NIDDM. Because the incidence of diabetes is high in
families of persons with NIDDM, a strong genetic pre-disposition is suspected.
However, NIDDM is most likely a polygenic disease, involving multiple genetic
predispositions to the development of the diabetic state.
The three major metabolic
abnormalities that con-tribute to hyperglycemia in NIDDM are defective
glucose-induced insulin secretion, increased hepatic glu-cose output, and
inability of insulin to stimulate glucose uptake in peripheral target tissues.
These abnormalities also involve the cellular glucose transport in cells,
liver, adipose tissue, and skeletal muscle, and they may be the result of
alterations in GLUTs. Another essential prob-lem in NIDDM may be reduced
sensitivity of fat and muscle cells to the effects of insulin (i.e., insulin resist-ance). Consequently, in
early stages of NIDDM, the pan-creas may produce normal or even excessive
amounts of insulin and only become impaired at insulin production at a later
stage of the disease. Recently, a hormone pro-duced in adipose tissue, resistin, has been identified and is
postulated to cause many of the derangements that ul-timately result in insulin
resistance.
Several putative sites of
insulin resistance have been identified in humans, including a defective
binding of in-sulin to a receptor and a blunting of insulin signal
trans-duction. Conditions associated with elevated insulin lev-els (hyperinsulinism), such as obesity, may
be the result of down-regulation in
the number of insulin receptors, effectively resulting in a state of insulin
resistance. Conversely, decreases in insulin levels (e.g., diabetes) may lead
to an up-regulation of the receptors,
which may shift the insulin dose–response curve to the left; that is, less
insulin would be required to produce a given bio-logical effect. The extent to
which receptor regulation actually participates in adjustments to changing
physio-logical conditions has not been definitively established.
Insulin resistance also has
been associated with a number of hormonal and metabolic states, including
Cushing’s syndrome (excessive corticosteroids), acro-megaly (excessive growth
hormone), and gestational di-abetes. Physiological or psychological stress also
can contribute to insulin resistance. Gestational
diabetes mellitus is a condition
that develops during the second trimester
of pregnancy; the cause may be rises in human placental lactogen and other
hormones that contribute to insulin resistance. This condition usually resolves
dur-ing the postpartum period. Another relatively common form of insulin
resistance is often seen in women with polycystic
ovarian syndrome, a disorder that is associ-ated with hyperandrogenism,
hirsutism, menstrual ir-regularities, obesity, and infertility.
Related Topics