Chapter: Medical Surgical Nursing: Assessment and Management of Problems Related to Male Reproductive Processes
Conditions Affecting the Testes and Adjacent Structures
Conditions Affecting the Testes and
Adjacent Structures
UNDESCENDED TESTIS (CRYPTORCHIDISM)
Cryptorchidism is a congenital condition characterized by fail-ure of one or both of
the testes to descend into the scrotum. One or both testes may be absent. The
testis may be located in the ab-dominal cavity or inguinal canal. If the testis
does not descend as the boy matures, a surgical procedure known as orchiopexy
is per-formed to position it properly. An incision is made over the inguinal
canal, and the testis is brought down and anchored in the scrotum.
ORCHITIS
Orchitis is an inflammation of the testes (testicular congestion)caused by
pyogenic, viral, spirochetal, parasitic, traumatic, chem-ical, or unknown
factors. Mumps is one such factor. Mumps vac-cination is recommended for
postpubertal men who have not been infected. When postpubertal men contract
mumps, about one in five develops some form of orchitis 4 to 7 days after the
jaw and neck swell. The testis may show some atrophy. In the past, sterility
and impotence often resulted. Today, a man who has never had mumps and who is
exposed to the disease receives gamma-globulin immediately; the disease is
likely to be less se-vere, with minimal or no complications.
Medical Management
If the cause of orchitis is bacterial, viral,
or fungal, therapy is di-rected at the specific infecting organism. Rest,
elevation of the scrotum, ice packs to reduce scrotal edema, antibiotics,
analgesic agents, and anti-inflammatory medications are recommended.
EPIDIDYMITIS
Epididymitis is an infection of the epididymis that usually de-scends from an
infected prostate or urinary tract. It may also de-velop as a complication of
gonorrhea. In men younger than age 35, the major cause of epididymitis is Chlamydia trachomatis. The in-fection
passes upward through the urethra and the ejaculatory duct and then along the
vas deferens to the epididymis.
The
patient complains of unilateral pain and soreness in the inguinal canal along
the course of the vas deferens and then de-velops pain and swelling in the
scrotum and the groin. The epi-didymis becomes swollen and extremely painful;
the patient’s temperature is elevated. The urine may contain pus (pyuria) and
bacteria (bacteriuria), and the patient may experience chills and fever.
Medical Management
If the patient is seen within the first 24
hours after onset of pain, the spermatic cord may be infiltrated with a local
anesthetic agent to relieve pain. If the epididymitis is from a chlamydial
infection, the patient and his sexual partner must be treated with
antibi-otics. The patient is observed for abscess formation as well. If no improvement occurs
within 2 weeks, an underlying testicular tumor should be considered. An
epididymectomy (excision of the epididymis from the testis) may be performed
for patients with recurrent, incapacitating episodes of epididymitis or for
those with chronic, painful conditions. With long-term epididymitis, the
passage of sperm may be obstructed. If the obstruction is bi-lateral,
infertility may result.
Nursing Management
The patient is placed on bed rest, and the
scrotum is elevated with a scrotal bridge or folded towel to prevent traction
on the sper-matic cord and to promote venous drainage and relieve pain.
Anti-microbial agents are administered as prescribed until the acute
inflammation subsides. Intermittent cold compresses to the scro-tum may help
ease the pain. Later, local heat or sitz baths may help resolve the
inflammation. Analgesic medications are admin-istered for pain relief as
prescribed.
The nurse instructs the patient to avoid
straining, lifting, and sexual stimulation until the infection is under
control. He should continue taking analgesic agents and antibiotics as
prescribed and using ice packs if necessary to relieve discomfort. He needs to
know that it may take 4 weeks or longer for the epididymis to re-turn to
normal.
TESTICULAR CANCER
Testicular cancer is the most common cancer in men 15 to35
years of age. Although testicular cancer occurs most often be-tween the ages of
15 and 40, it can occur in males of any age. It is a highly treatable and
usually curable form of cancer. An es-timated 7,500 men are diagnosed with
testicular cancer each year, and approximately 400 die from testicular cancer
annually (American Cancer Society, 2002).
The testicles contain several types of cells,
each of which may develop into one or more types of cancer. The type of cancer
de-termines the appropriate treatment and affects the prognosis. Testicular
cancers are classified as germinal or nongerminal (stro-mal); secondary
testicular cancers may also occur.
Germinal Tumors
Over 90% of all cancers of the testicle are
germinal; geminal tumors may be further classified as seminomas or
nonseminomas. About half of all geminal tumors are seminomas, or tumors that
develop from the sperm-producing cells of the testes. Nonseminoma ger-minal
cell tumors tend to develop earlier in life than seminomas, usually occurring
in men in their 20s. Examples of nonseminomas include teratocarcinomas,
choriocarcinomas, yolk sac carcino-mas, and embryonal carcinomas. Seminomas
tend to remain lo-calized, whereas nonseminomatous tumors grow quickly.
Nongerminal Tumors
Testicular cancer may also develop in the
supportive and hormone-producing tissues, or stroma, of the testicles. These
tumors ac-count for about 4% of testicular tumors in adults and 20% of
testicular tumors in children. The two main types of stromal tu-mors are Leydig
cell tumors and Sertoli cell tumors. Although these tumors infrequently spread
beyond the testicle, a small number of these tumors metastasize and tend to be
resistant to chemotherapy and radiation therapy.
Secondary Testicular Tumors
Secondary testicular tumors are those that
have metastasized to the testicle from other organs. Lymphoma is the most
common cause of secondary testicular cancer. Cancers may also spread to the
testicles from the prostate gland, lung, skin (melanoma), kid-ney, and other organs.
The prognosis for these cancers is usually poor because these cancers generally
also spread to other organs. Treatment depends on the specific type of cancer
(American Cancer Society, 2002).
Risk Factors
The risk for testicular cancer is several
times greater in men with any type of undescended testis than in the general
population (Bosl, Bajorin, Scheinfeld et al., 2001). Risk factors include a
family history of testicular cancer and cancer of one testicle, which increases
the risk for the other testicle. Race and ethnicity have been identified as
risk factors: Caucasian American men have a five times greater risk than that
of African American men and more than double the risk of Asian American men.
Occupational hazards, including exposure to chemicals encountered in mining,
oil and gas production, and leather processing, have been sug-gested as
possible risk factors. Prenatal exposure to DES may also be a risk factor, but
evidence is not strong (American Cancer Society, 2002). Vasectomy, once
considered a possible risk factor, has been shown in recent studies not to be a
risk factor (Cox, Sneyd, Paul et al., 2002).
Clinical Manifestations
The symptoms appear gradually, with a mass or
lump on the tes-ticle and generally painless enlargement of the testis. The
patient may complain of heaviness in the scrotum, inguinal area, or lower
abdomen. Backache (from retroperitoneal node extension), ab-dominal pain,
weight loss, and general weakness may result from metastasis. Enlargement of
the testis without pain is a significant diagnostic finding. Testicular tumors
tend to metastasize early, spreading from the testis to the lymph nodes in the
retroperi-toneum and to the lungs.
Assessment and Diagnostic Findings
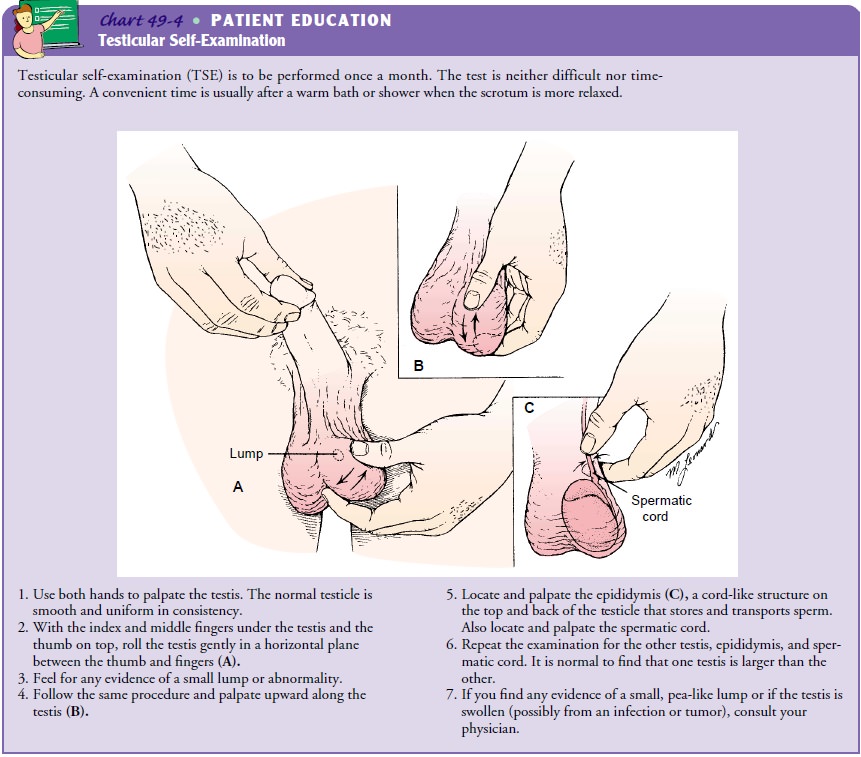
Monthly testicular self-examinations (TSEs)
are effective in de-tecting testicular cancer (Chart 49-4). Teaching men of all
ages to perform TSE is an important health promotion intervention for early
detection of testicular cancer. Since testicular cancer oc-curs most often in
young adults, testicular self-examination should begin during adolescence.
Human chorionic gonadotropin and alpha-fetoprotein are tumor markers that may be elevated in patients with testicular cancer. (Tumor markers are substances synthesized by the tumor cells and released into the circulation in abnormal amounts.) Tumor marker levels in the blood are used for diagnosis, staging, and monitoring the response to treatment. Other diagnostic tests include intravenous urography to detect any ureteral devi-ation caused by a tumor mass; lymphangiography to assess the extent of tumor spread to the lymphatic system; ultrasound to determine the presence and size of the testicular mass; and CT scan of the chest, abdomen, and pelvis to determine the extent of the disease in the lungs, retroperitoneum, and pelvis. Micro-scopic analysis of tissue is the only definitive way to determine if cancer is present but is usually performed at the time of surgery rather than as a part of the diagnostic workup to reduce the risk of promoting spread of the cancer (American Cancer Society, 2000).
Medical Management
Testicular cancer is one of the most curable
solid tumors. The goals of management are to eradicate the disease and achieve
a cure. Treatment selection is based on the cell type and the anatomic extent
of the disease. The testis is removed by orchi-ectomy through an inguinal
incision with a high ligation of the spermatic cord. A gel-filled prosthesis
can be implanted. After unilateral orchiectomy for testicular cancer, most patients
expe-rience no impairment of endocrine function. Other patients, however, have
decreased hormonal levels, suggesting that the un-affected testis is not
functioning at normal levels. Retroperitoneal lymph node dissection to prevent
lymphatic spread of the cancer may be performed after orchiectomy. Although
libido and or-gasm are usually unimpaired after retroperitoneal lymph node
dissection, the patient may develop ejaculatory dysfunction with resultant
infertility. Thus, sperm banking before surgery may be considered (Agarwa,
2000; Zapzalka et al., 1999).
Postoperative
irradiation of the lymph nodes from the di-aphragm to the iliac region is used
in treating seminomas. Radi-ation is delivered only to the affected side; the
other testis is shielded from radiation to preserve fertility. Radiation is
also used for patients whose disease does not respond to chemotherapy or for
whom lymph node surgery is not recommended. Lymphan-giograms and CT scans are
used to determine spread of the dis-ease to the lymph nodes.
Testicular
carcinomas are highly responsive to chemotherapy. (Bosl et al., 2001)
Chemotherapy with cisplatin-based regimens results in a high percentage of
complete remissions. Good results may be obtained by combining different types
of treatment, in-cluding surgery, radiation therapy, and chemotherapy. Even
with disseminated testicular cancer, the prognosis is favorable, and the
disease is probably curable because of advances in diagnosis and treatment.A
patient with a history of one testicular tumor has a greater chance of
developing subsequent tumors. Follow-up studies in-clude chest x-rays,
excretory urography, radioimmunoassay of human chorionic gonadotropins and
alpha-fetoprotein levels, and examination of lymph nodes to detect recurrent malignancy.
Long-term side effects associated with
treatments for testicu-lar cancer include kidney damage, hearing problems,
gonadal damage, neurological changes, and rarely secondary cancers
(Kollmannsberger, Kuzcyk, Mayer et al., 1999). Research on treatment regimens
with less toxicity and the use of cytoprotec-tants is ongoing.
Nursing Management
Nursing management includes assessment of the
patient’s physi-cal and psychological status and monitoring the patient for
re-sponse to and possible effects of surgery, chemotherapy, and radiation
therapy. In addition, be-cause the patient may have difficulty coping with his
condition, issues related to body image and sexuality are addressed. He needs
encouragement to maintain a positive attitude during what may be a long course
of therapy. He also needs to know that radiation therapy will not necessarily
prevent him from fathering children, nor does unilateral excision of a testis
necessarily decrease virility. The nurse reminds the patient about the
importance of perform-ing TSE and keeping follow-up appointments with the
physician. The patient is also encouraged to participate in health promotion
and health screening activities.
HYDROCELE
A hydrocele is a collection of fluid,
generally in the tunica vagi-nalis of the testis, although it may also collect
within the sper-matic cord. The tunica vaginalis becomes widely distended with
fluid. Hydrocele can be differentiated from a hernia by transillu-mination; a
hydrocele transmits light, whereas a hernia does not. Hydrocele may be acute or
chronic. Acute hydrocele may occur in association with acute infectious
diseases of the epididymis or as a result of local injury or systemic
infectious diseases, such as mumps. The cause of chronic hydrocele is unknown.
Usually, therapy is not required. Treatment
is necessary only if the hydrocele becomes tense and compromises testicular
circu-lation or if the scrotal mass becomes large, uncomfortable, or
em-barrassing. In the surgical treatment of hydrocele, an incision is made through
the wall of the scrotum down to the distended tu-nica vaginalis. The sac is
resected or, after being opened, is su-tured together to collapse the wall.
Postoperatively, the patient wears an athletic supporter for comfort and
support. The major complication is hematoma in the loose scrotal tissues.
VARICOCELE
A varicocele
is an abnormal dilation of the veins of the pampini-form venous plexus in the
scrotum (the network of veins from the testis and the epididymis that
constitute part of the spermatic cord). Varicoceles usually occur in the veins
on the upper portion of the left testicle in adults. In some men, a varicocele
has been associated with infertility. Few, if any, subjective symptoms may be
produced by the enlarged spermatic vein, and no treatment is required unless
fertility is a concern. Symptomatic varicocele (pain, tenderness, and
discomfort in the inguinal region) is corrected surgically by ligat-ing the
external spermatic vein at the inguinal area. An ice pack may be applied to the
scrotum for the first few hours after surgery to relieve edema. The patient
then wears a scrotal supporter.
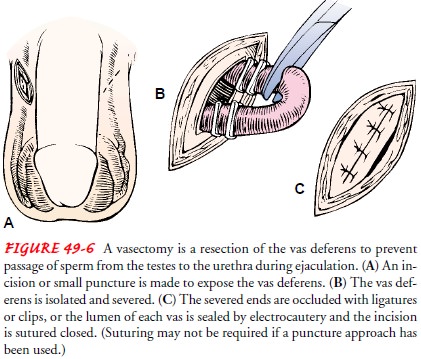
VASECTOMY
Vasectomy, or male sterilization, is the ligation and transection ofpart of the
vas deferens, with or without removal of a segment of the vas deferens. To
prevent the passage of the sperm from the testes, the vas deferens is exposed
through a surgical opening in the scrotum or a puncture using a sharp, curved
hemostat (Fig. 49-6). The severed ends are occluded with ligatures or clips, or
the lumen of each vas deferens is sealed by cautery. The spermatozoa, which are
manufactured in the testes, cannot travel up the vas deferens after this
surgery.
Because
seminal fluid is manufactured predominantly in the seminal vesicles and
prostate gland, which are unaffected by va-sectomy, no noticeable decrease
occurs in the amount of ejacu-late even though it contains no spermatozoa.
Because the sperm cells have no exit, they are resorbed into the body. This
procedure has no effect on sexual potency, erection, ejaculation, or
produc-tion of male hormones and provides no protection against sexu-ally
transmitted diseases.
Couples who were worried about pregnancy
resulting from contraceptive failure often report a decrease in concern and an
in-crease in spontaneous sexual arousal after vasectomy. Concise and factual
preoperative explanations may minimize or relieve the pa-tient’s concerns
related to masculinity. Although a relationship between vasectomy and
autoimmune disorders and prostatic can-cer has been suggested, there is no
clinical evidence of either.
The
patient is advised that he will be sterile but that potency will not be altered
after a bilateral vasectomy. As with any surgi-cal procedure, a surgical
consent form must be signed. On rare occasions, a spontaneous reanastomosis of
the vas deferens oc-curs, making it possible to impregnate a partner.
Complications of vasectomy include scrotal
ecchymoses and swelling, superficial wound infection, vasitis (inflammation of
the vas deferens), epididymitis or epididymo-orchitis, hematomas, and spermatic
granuloma. A spermatic granuloma is an inflammatory response to the collection
of sperm leaking into the scrotum from the severed end of the proximal vas
deferens. This can initiate re-canalization of the vas deferens, making
pregnancy possible.
Nursing Management
Ice
bags are applied intermittently to the scrotum for several hours after surgery
to reduce swelling and to relieve discomfort. The nurse advises the patient to
wear cotton, Jockey-type briefs for added comfort and support. He may become
greatly con-cerned about the discoloration of the scrotal skin and superficial
swelling. These are temporary conditions that occur frequently after vasectomy
and may be relieved by sitz baths.
Sexual
intercourse may be resumed as desired, although fer-tility remains for a
varying time after vasectomy until the sper-matozoa stored distal to the
severed vas deferens have been evacuated. Other methods of contraception should
be used until infertility is confirmed by an examination of ejaculate. Some
physicians examine a specimen 4 weeks after the vasectomy to determine
sterility; others examine two consecutive specimens 1 month apart; and still
others consider a patient sterile after 36 ejaculations.
Vasovasostomy (Sterilization Reversal)
Microsurgical techniques are used to reverse
a vasectomy (vaso-vasostomy), thus restoring patency to the vas deferens. Many
men have sperm in their ejaculate after a reversal, and 40% to 75% can
impregnate a partner.
Banking Sperm
Storing fertile semen in a sperm bank before
a vasectomy is an op-tion for men who face an unforeseen life event that may
cause them to want to father a child at a later time. In addition, if a man is
about to undergo a procedure or treatment (eg, radiation ther-apy to the pelvis
or chemotherapy) that may affect his fertility, sperm banking may be
considered. This procedure usually re-quires several visits to the facility
where the sperm is stored under hypothermic conditions. The semen is produced
by masturba-tion and collected in a sterile container for storage.
Related Topics