Chapter: Medical Immunology: Systemic Lupus Erythematosus
Clinical Manifestations - Systemic Lupus Erythematosus
CLINICAL MANIFESTATIONS
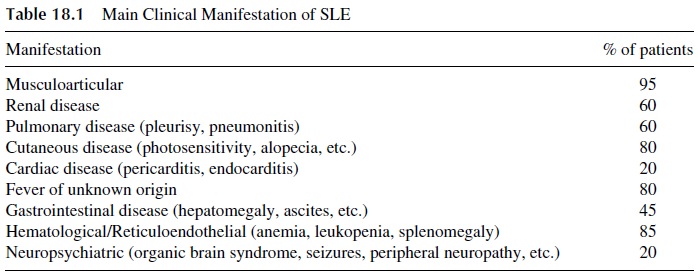
The clinical expression of SLE varies among different patients. The kind of organ (vital vs. nonvital) that becomes involved determines the seriousness and the overall prognosis of the disease. The average frequency of some main clinical manifestations of SLE that may be observed during the entire course of SLE is shown in Table 18.1.
A. Diagnosis
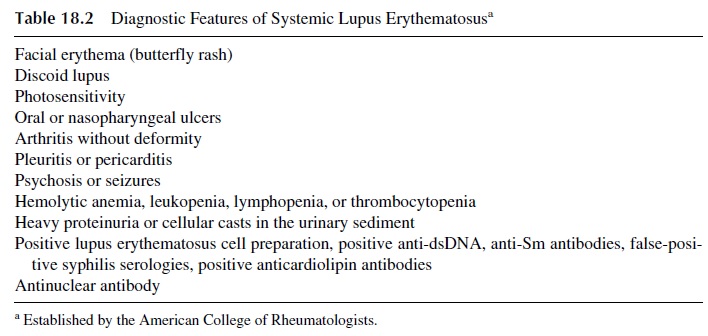
The diagnosis is based on the verification that any four of the clinical and/or laboratory manifestations listed in Table 18.2 are present simultaneously or serially during a period of observation.
B.Course
Exacerbations and remissions, heralded by the appearance of new manifestations and wors-ening of preexisting symptoms, give the disease its fluctuating natural history. Although high levels of autoantibodies and low levels of serum complement (C3, C4) may accom-pany clinical disease activity, there is no laboratory marker as of yet that can reliably pre-dict an upcoming flare.
C. Overlap Syndromes
Occasionally, physicians observe clinical situations in which the differentiation between SLE and another connective tissue disease is difficult. In some patients the distinction may be impossible, and they are classified as having an overlap syndrome.
This syndrome rep-resents the association of SLE with another disorder such as scleroderma or rheumatoid arthritis. On the other hand, some patients have symptoms and laboratory findings that are reminiscent of lupus, yet a formal diagnosis (defined by the criteria listed in Table 18.2) cannot be made. Patients who take certain drugs (hydralazine, procainamide, etc.) may pre-sent with an incomplete picture of lupus known as drug-induced lupus. Other patients may present with an incomplete picture of lupus that may remain stable over a period of years or evolve with the appearance of additional manifestations.
Related Topics