Chapter: Medical Immunology: Systemic Lupus Erythematosus
Immunological Abnormalities in SLE(Systemic Lupus Erythematosus)
IMMUNOLOGICAL ABNORMALITIES IN SLE
A. Autoantibodies
The LE cell is a peculiar-looking polymorphonuclear leukocyte, which has ingested nuclear material. It was possible to reproduce this phenomenon in vitro by incubating normal neutrophils with damaged leukocytes preincubated with sera obtained from SLE patients. Investigations concerning the nature of this phenomenon led to the discovery that antibod-ies directed to nuclei could promote the formation of LE cells and subsequently to the def-inition of a heterogeneous group of antinuclear antibodies.
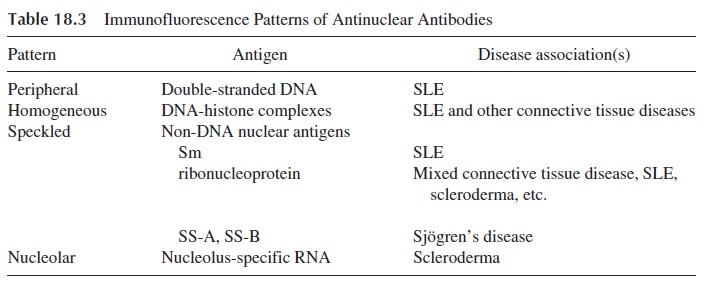
Antinuclear antibodies (ANAs) are detected by an indirect immunofluorescence as-say using a variety of tissues and cell lines as substrates. A positive result is indicated by the observation of nuclear fluorescence after incubating the cells with the patient’s serum and, after thorough washing to remove unbound immunoglobulins, with an antihuman im-munoglobulin serum. Four patterns of fluorescence can be seen indicating different types of antinuclear antibodies (see Table 18.3). The test for antinuclear antibodies is not very specific but is very sensitive. A negative result virtually excludes the diagnosis of SLE (95% of patients with SLE are ANA positive), while high titers are strongly suggestive of SLE but not confirmatory, since ANAs can be detected in other conditions including other systemic autoimmune/collagen diseases and chronic infections.
DNA antibodies are the most important in SLE. They can react with single-stranded DNA (ssDNA) or with double-stranded DNA (dsDNA). Two thirds of patients with SLE have circulating anti-DNA antibodies. Although anti-ssDNA may be found in many diseases besides SLE, anti-dsDNA antibodies are found almost exclusively in SLE (40–60% of the patients).
Most are commonly detected by immunofluorescence using as a substrate a noninfectious flagellate,Crithidia lucilliae, which has a kinetoplast packed with double-stranded DNA . This test is very specific, and the antibodies can be semi-quantitated by titration of the serum (to determine the highest serum dilution associated with visible fluorescence of the kinetoplast after addition of a fluorescent-labeled anti-IgG antibody). Most laboratories use enzyme-linked immunosorbent assays to detect DNA antibodies.
Antibodies to the DNA-histone complex are present in over 65% of patients with SLE. The use of enzyme-linked immunosorbent assays (ELISAs) has permitted the identi-fication of antibodies to all histone proteins including H1, H2A, H2B, H3, and H4. Antihi-stone antibodies are also present in patients with drug-induced SLE, most frequently asso-ciated with hydralazine and procainamide therapies.
Antibodies to nonhistone proteins have been studied intensely lately. The nonhis-tones against which antibodies have been described include:
· Anti-Sm. Antibodies to the Sm antigen are present in one third of patients with SLE.Sm antibodies have not been found in other conditions. The antigenic determi-nant is on a protein that is conjugated to one of six different small nuclear RNAs (snRNA).
· Anti-U1-RNP.The antigenic epitope is on a protein conjugated to U1-RNA. Anti-bodies to this antigen are present in the majority of patients with SLE and in mixed connective tissue disease, which represents an overlap syndrome.
· Anti-SS-A/Ro.These antibodies are present in one third of patients with SLE and twothirds of patients with Sjögren’s syndrome (SS). Antibodies to the Ro antigen are frequently found in patients with SLE who are ANA-negative. Babies born to mothers with Ro antibodies may have heart block, leukopenia, and/or skin rash.
· Anti-SS-B/La.The antigenic epitope recognized by this antibody is on a 43 kDa pro-tein conjugated to RNA. Antibodies to La antigen are present in about one third of patients with SLE and in approximately one half of the patients with Sjö-gren’s syndrome.
Patients with SLE frequently have antiphospholipid antibodies and anticardiolipin antibodies. The anticardiolipin antibodies recognize a cryptic epitope on β2-glycoprotein I that is exposed after it binds to anionic phospholipids. A related group of antibodies are the phospholipid antibodies that react with phospholipids and are apparently implicated as one of the causes of clotting disorders in SLE.
SLE patients may present with bleeding disorders, which in some cases are secondary to autoimmune thrombocytopenia and in others seem to be caused by heterogeneous col-lection of antibodies to clotting factors, known as lupus anticoagulant. Some of these anti-bodies seem to recognize complexes of phospholipids and clotting factors (e.g., prothrom-bin), thus overlapping with the phospholipid antibodies.
B. The Pathogenic Role of Autoantibodies in SLE
Classically, it has been accepted that autoantibodies do not play the initiating role in the pathogenesis of SLE. On the other hand, it is accepted that autoantibodies are likely to ei-ther play an important role as cofactors in the pathogenesis of the disease or play a direct role in the pathogenesis of some of the manifestations of the disease. This dogma, based on the belief that autoantibodies cannot enter living cells, has recently been challenged. Not only can anti-RNP, anti-DNA, and anti-Ro enter live cells, but they also can induce apop-tosis. Thus, the concepts about the pathogenic role of autoantibodies are likely to change in the future.
1. T-cell antibodies are believed to bind and eliminate certain subsets of T cells (suppressor-inducer); as a consequence, the normal negative feedback circuits controlling B-cell activity may not be operational, explaining the uncontrolled production of autoantibodies by the B cells.
2. Antibodies against CR1 (complement receptor 1) and against the C3 convertase are occasionally detected. CR1 antibodies may block the receptor and interfere with the clearance of immune complexes. Antibodies to the C3 convertase, by stimulating its function, may contribute to increased C3 consumption.
3. Anti–red cell antibodies and antiplatelet antibodies are the cause, respectively, of hemolytic anemia and thrombocytopenia.
4. Autoantibodies directed against central nervous system (CNS) antigens may be detected in the serum and the cerebrospinal fluid of patients with SLE who have CNS involvement and have also been considered, but not proven, pathogenic.
5. DNA antibodies form immune complexes by reacting with DNA and are impli-cated in the pathogenesis of glomerulonephritis .
6. Cardiolipin antibodies, phospholipid antibodies, and lupus anticoagulant are de-tected frequently in SLE patients. The cardiolipin antibodies cause false positiv-ity in serological tests for syphilis. Cardiolipin and phospholipid antibodies are also associated with miscarriages, thrombophlebitis, thrombocytopenia, and var-ious central nervous system manifestations secondary to vascular thrombosis. The constellation of these symptoms is known as phospholipid antibody syn-drome, and although it was first recognized in lupus patients, the majority of the cases do not fulfill the diagnostic criteria for SLE.
7. Ro antibodies, when present in mothers with SLE, seem to be associated with the development of heart block in their babies.
C. The Diagnostic Value of Autoantibodies
Some autoantibodies may not be linked with any specific clinical manifestations but are very useful as disease markers. For example, dsDNA and Sm antibodies are diagnostic of SLE. Most other autoantibodies are present in more than one clinical disease or syndrome. However, even if many of the patients share some common immunological abnormalities, particularly the presence of antinuclear antibodies or of rheumatoid factor, specific disor-ders can usually be individualized by the presence of a specific set of autoantibodies.
Related Topics