Chapter: Medical Immunology: Immunohematology
Blood Transfusion Reactions
BLOOD TRANSFUSION REACTIONS
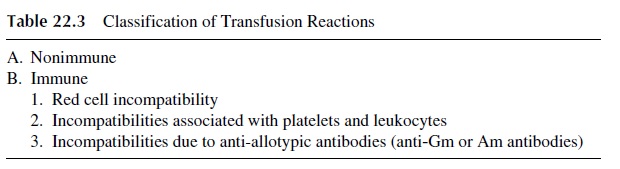
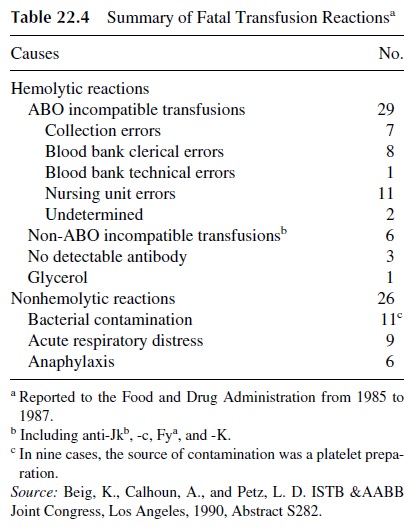
Transfusion reactions may occur due to a wide variety of causes (Table 22.3). Among them, the most severe are those associated with hemolysis, which may be life threatening. A list of the causes of fatal transfusion reactions reported to the U.S. FDA from 1985 to 1987 is reproduced in Table 22.4.
The most frequent cause is an ABO mismatch due to clerical error, resulting in trans-fusion of the wrong blood. Transfusion of blood incompatible for other blood groups to a patient previously sensitized during pregnancy or as a consequence of earlier transfusions can also cause a hemolytic reaction.
A. Intravascular Hemolytic Reactions
The binding of preformed IgM antibodies to the red cells triggers intravascular hemolytic transfusion reactions. IgM antibodies are very effective in causing the activation of the complement system. Massive complement activation by red cell antibodies causes intravascular red cell lysis, with release of hemoglobin into the circulation. Most intravascu-lar reactions are due to ABO incompatibility. The direct antiglobulin test may be negative if donor cells are quickly lysed.
Due to the massive release of soluble complement fragments (e.g., C3a and C5a) with anaphylotoxic properties, the patient may suffer generalized vasodilatation, hypotension, and shock. Because of the interrelationships between the complement and clotting systems, disseminated intravascular coagulation may occur during a severe transfusion reaction. As a consequence of the nephrotoxicity of free hemoglobin, the patient may develop acute re-nal failure, usually due to acute tubular necrosis.
B. Extravascular Hemolytic Reactions
Extravascular hemolytic reactions are caused by the opsonization of red cells with IgG an-tibodies. IgG red cell antibodies can activate complement but do not cause spontaneous red cell lysis. Red cells opsonized with IgG (often with associated C3b) are efficiently taken up and destroyed by phagocytic cells, particularly splenic and hepatic macrophages.
These reactions are usually less severe than intravascular transfusion reactions. In ad-dition, transfusion reactions may be delayed when an anamnestic response in a patient with undetectable antibody is the precipitating factor. Typically, a positive direct antiglobulin (Coombs’) test will be noted after transfusion in association with a rapidly diminishing red cell concentration.
C. Clinical Presentation
The most common initial symptom in a hemolytic transfusion reaction is fever, frequently associated with chills. Red or wine-colored urine (due to hemoglobinuria) may be noted. With progression of the reaction, the patient may experience chest pains, dyspnea, hy-potension, and shock. Renal damage is indicated by back pain, oliguria, and in most severe cases, anuria.
During surgery, the only symptom may be bleeding and/or hypotension. Generalized bleeding is the most serious manifestation of disseminated intravascular coagulation
D. Laboratory Investigation
Immediately after a hemolytic transfusion reaction is suspected, the following procedures must be carried out:
· A clerical check to detect any errors that may have resulted in the administration of a unit of blood to the wrong patient.
· Confirmation of intravascular hemolysis by visual or photometric comparison of pre-and postreaction plasma specimens for free hemoglobin (the prereaction spec-imen should be light yellow, and the postreaction sample should have a pink/red discoloration).
· Direct antiglobulin (Coombs’) test on pre- and postreaction blood samples.
If any of the above procedures gives a positive result supporting a diagnosis of intravascu-lar hemolysis, additional serological investigations are indicated, including the following:
· Repeat ABO and Rh typing on patient and donor samples. Repeat antibody screening and cross-matching.
· If an anti–red cell antibody is detected, determine its specificity using a red cell panel in which group O red cells of varied antigenic composition are incubated with the patient’s serum to determine which RBC antigen(s) are recognized by the patient’s antibody(ies).
Additionally, one or several of the following confirmatory tests may be performed:
· Measurement of unconjugated bilirubin on blood drawn 5–7 hours after transfusion (the concentration should rise as the released hemoglobin is processed).
· Determination of free hemoglobin and/or hemosiderin in the urine (neither is nor-mally detected in the urine).
· Measurement of serum haptoglobin (if hemolysis is not apparent upon visual inspec-tion of the serum).
E. Nonhemolytic Immune Transfusion Reactions
1. Antileukocyte Antibodies
When a patient has antibodies directed to leukocyte antigens, a transfusion of any blood product containing cells expressing those antigens can elicit a febrile transfusion reaction. Leukocyte-depleted blood products should be used for transfusions in patients with recur-rent febrile reactions.
Special problems are presented by patients requiring platelet concentrates that have developed anti-HLA antibodies or antibodies directed to platelet-specific antigens (HPA antigens). In such cases, it will be necessary to give HLA or HPA-matched platelets, since platelets will be rapidly destroyed if given to a sensitized individual with circulating anti-bodies to the antigens expressed by the donor’s platelets.
Transfusion of blood products containing antibodies to leukocyte antigens expressed by the patient receiving the transfusion can induce intravascular leukocyte aggregation. These aggregates are usually trapped in the pulmonary microcirculation, causing acute res-piratory distress and, in some cases, noncardiogenic pulmonary edema. A similar situation may emerge when granulocyte concentrates are given to a patient with antileukocyte anti-bodies reactive with the transfused granulocytes.
2. Anti-IgA Antibodies
The transfusion of any IgA-containing blood product into a patient with preformed anti-IgA antibodies can cause an anaphylactic transfusion reaction. Transfusion reactions are not usually observed when the antibody titers (determined by passive hemagglutination) are low. Anti-IgA antibodies are mostly detected in immunodeficient individuals, particu-larly those with IgA deficiency.
It is very important to test for anti-IgA antibodies in any patient with known IgA de-ficiency that is going to require a transfusion, even if the patient has never been previously transfused. If an anti-IgA antibody is detected, it is important to administer packed red cells with all traces of plasma removed by extensive washing. If plasma products are needed, they should be obtained from IgA-deficient donors.
Related Topics