Chapter: Psychiatric Mental Health Nursing : Anxiety, Anxiety Disorders, and Stress-Related Illness
Anxiety as a Response to Stress
ANXIETY AS A RESPONSE TO STRESS
Stress is the wear and tear that
life causes on the body (Selye,
1956). It occurs when a person has difficulty deal-ing with life situations,
problems, and goals. Each person handles stress differently: One person can
thrive in a situ-ation that creates great distress for another. For example,
many people view public speaking as scary, but for teach-ers and actors, it is
an everyday, enjoyable experience. Marriage, children, airplanes, snakes, a new
job, a new school, and leaving home are examples of stress-causing events.
Hans Selye (1956, 1974), an endocrinologist, identified the physiologic
aspects of stress, which he labeled the gen-eral
adaptation syndrome. He used laboratory animals to assess biologic system changes; the stages of the body’s physical
responses to pain, heat, toxins, and restraint; and, later, the mind’s
emotional responses to real or perceived stressors. He determined three stages
of reaction to stress:
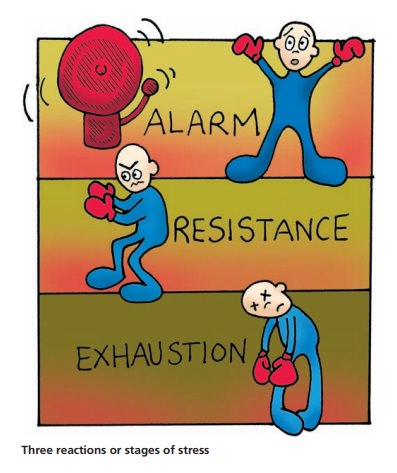
In the alarm reaction stage,
stress stimulates the body to send messages from the hypothalamus to the glands
(such as the adrenal gland, to send out adrenaline and norepinephrine for fuel)
and organs (such as the liver, to reconvert glycogen stores to glucose for
food) to pre-pare for potential defense needs.
·
In the resistance stage,
the digestive system reduces function to shunt blood to areas needed for
defense. The lungs take in more air, and the heart beats faster and harder so
it can circulate this highly oxygenated and highly nourished blood to the
muscles to defend the body by fight, flight, or freeze behaviors. If the
per-son adapts to the stress, the body responses relax, and the gland, organ,
and systemic responses abate.
·
The exhaustion stage
occurs when the person has re-sponded negatively to anxiety and stress: body
stores are depleted or the emotional components are not re-solved, resulting in
continual arousal of the physiologic responses and little reserve capacity.
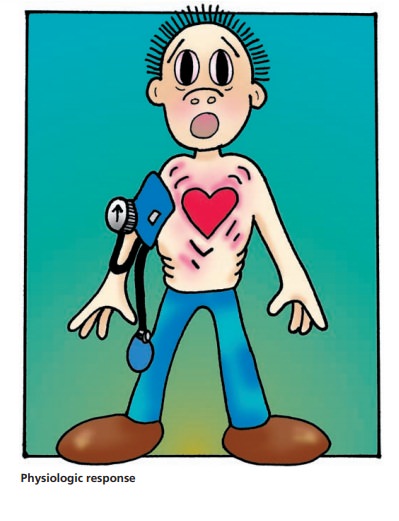
Autonomic nervous system responses to fear and anxi-ety generate
the involuntary activities of the body that are involved in self-preservation.
Sympathetic nerve fibers “charge up” the vital signs at any hint of danger to
prepare the body’s defenses. The adrenal glands release adrenalin
(epinephrine), which causes the body to take in more oxy-gen, dilate the
pupils, and increase arterial pressure and heart rate while constricting the
peripheral vessels and shunting blood from the gastrointestinal and
reproductive systems and increasing glycogenolysis to free glucose for fuel for
the heart, muscles, and central nervous system. When the danger has passed,
parasympathetic nerve fibers reverse this process and return the body to normal
operat-ing conditions until the next sign of threat reactivates the sympathetic
responses.
Anxiety causes uncomfortable cognitive, psychomotor, and
physiologic responses, such as difficulty with logical thought, increasingly
agitated motor activity, and elevated vital signs. To reduce these
uncomfortable feelings, the person tries to reduce the level of discomfort by
imple-menting new adaptive behaviors or defense mechanisms. Adaptive behaviors
can be positive and help the person to learn, for example, using imagery
techniques to refocus attention on a pleasant scene, practicing sequential
relax-ation of the body from head to toe, and breathing slowly and steadily to
reduce muscle tension and vital signs. Neg-ative responses to anxiety can
result in maladaptive behav-iors such as tension headaches, pain syndromes, and
stress-related responses that reduce the efficiency of the immune system.
People can communicate anxiety to others both ver-bally and
nonverbally. If someone yells “fire,” others around them can become anxious as
they picture a fire and the possible threat that represents. Viewing a
distraught mother searching for her lost child in a shopping mall can cause
anxiety in others as they imagine the panic she is experiencing. They can
convey anxiety nonverbally through empathy, which is the sense of walking in
another person’s shoes for a moment in time (Sullivan, 1952).
Examples of nonverbal empathetic communication are when the family
of a client undergoing surgery can tell from the physician’s body language that
their loved one has died, when the nurse reads a plea for help in a client’s
eyes, or when a person feels the tension in a room where two people have been
arguing and are now not speaking to each other.
Levels of Anxiety
Anxiety has both healthy and harmful aspects depending on its
degree and duration as well as on how well the per-son copes with it. Anxiety
has four levels: mild, moderate, severe, and panic (Table 13.1). Each level
causes both physiologic and emotional changes in the person.
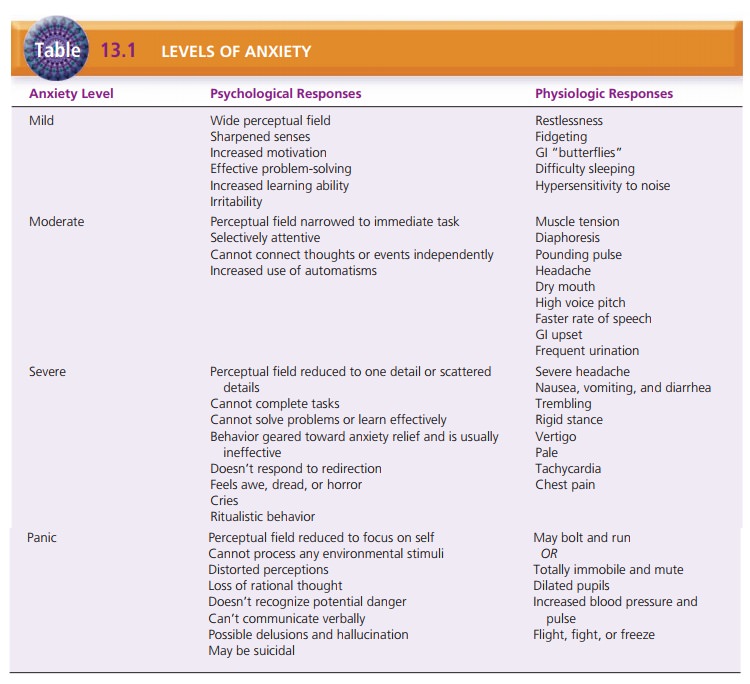
Mild anxiety is a sensation that something
is different and warrants special
attention. Sensory stimulation increases and helps the person focus attention
to learn, solve prob-lems, think, act, feel, and protect himself or herself.
Mild anxiety often motivates people to make changes or to engage in
goal-directed activity. For example, it helps students to focus on studying for
an examination.
Moderate anxiety is the disturbing feeling
that something is definitely wrong;
the person becomes nervous or agitated. In moderate anxiety, the person can
still process information, solve problems, and learn new things with assistance
fromothers. He or she has difficulty concentrating independently but can be
redirected to the topic. For example, the nurse might be giving preoperative
instructions to a client who is anxious about the upcoming surgical procedure.
As the nurse is teaching, the client’s attention wanders but the nurse can
regain the client’s attention and direct him or her back to the task at hand.
As the person progresses to severe
anxiety and panic, more primitive survival skills take over, defensive
responses ensue, and cognitive skills decrease significantly. A person with
severe anxiety has trouble thinking and reasoning. Muscles tighten and vital
signs increase. The person paces; is restless, irritable, and angry; or uses
other similar emotional–psychomotor means to release tension. In panic, the
emotional–psychomotor realm predominates with accompanying fight, flight, or
freeze responses. Adrenaline surge greatly increases vital signs. Pupils
enlarge to let in more light, and the only cognitive process focuses on the
person’s defense.
Working with Anxious Clients
Nurses encounter anxious clients and families in a wide variety of
situations such as before surgery and in emer-gency departments, intensive care
units, offices, and clin-ics. First and foremost, the nurse must assess the
person’s anxiety level because that determines what interventions are likely to
be effective.
Mild anxiety is an asset to the client and requires no direct
intervention. People with mild anxiety can learn and solve problems and are
even eager for information. Teach-ing can be very effective when the client is
mildly anxious.
In moderate anxiety, the nurse must be certain that the client is
following what the nurse is saying. The client’s attention can wander, and he
or she may have some difficulty concentrating over time. Speaking in short,
simple, and easy-to-understand sentences is effective; the nurse must stop to
ensure that the client is still taking in information correctly. The nurse may
need to redirect the client back to the topic if the client goes off on an
unrelated tangent.
When anxiety becomes severe, the client no longer can pay attention
or take in information. The nurse’s goal must be to lower the person’s anxiety
level to moderate or mild before proceeding with anything else. It is also
essential to remain with the person because anxiety is likely to worsen if he
or she is left alone. Talking to the client in a low, calm, and soothing voice
can help. If the person cannot sit still, walking with him or her while talking
can be effective. What the nurse talks about matters less than how he or she
says the words. Helping the person to take deep even breaths can help lower
anxiety.
During panic-level anxiety, the person’s safety is the pri-mary
concern. He or she cannot perceive potential harm and may have no capacity for
rational thought. The nurse must keep talking to the person in a comforting
manner, even though the client cannot process what the nurse is saying. Going
to a small, quiet, and nonstimulating envi-ronment may help to reduce anxiety.
The nurse can reas-sure the person that this is anxiety, that it will pass, and
that he or she is in a safe place. The nurse should remain with the client
until the panic recedes. Panic-level anxiety is not sustained indefinitely but
can last from 5–30 minutes.
When working with an anxious person, the nurse must be aware of his
or her own anxiety level. It is easy for the nurse to become increasingly
anxious. Remaining calm and in control is essential if the nurse is going to
work effectively with the client.
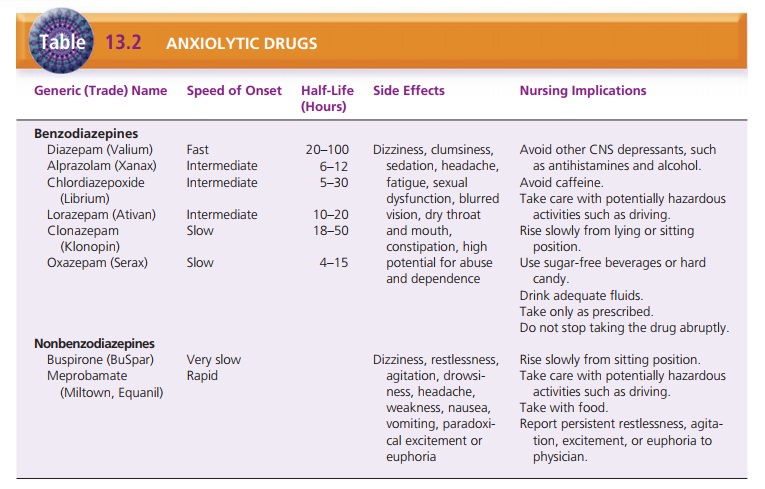
Short-term anxiety can be treated with anxiolytic medications
(Table 13.2). Most of these drugs are benzo-diazepines, which are commonly
prescribed for anxiety. Benzodiazepines have a high potential for abuse and
dependence, however, so their use should be short-term, ideally no longer than
4 to 6 weeks. These drugs are designed to relieve anxiety so that the person
can deal more effectively with whatever crisis or situation is caus-ing stress.
Unfortunately, many people see these drugs as a “cure” for anxiety and continue
to use them instead of learning more effective coping skills or making needed
changes.
Stress-Related Illness
Stress-related illness is a broad term that covers a spectrum of
illnesses that result from or worsen because of chronic, long-term, or
unresolved stress. Chronic stress that is repressed can cause eating disorders,
such as anorexia ner-vosa and bulimia. Repressed stress can cause physical
symptoms with no actual organic disease, called somatoform disorders . Stress
can also exacerbate the symptoms of many medical illness, such as hypertension
and ulcerative colitis. Chronic or recurrent anxiety resulting from stress may
also be diagnosed as an anxiety disorder.
OVERVIEW OF ANXIETY DISORDERS
Anxiety disorders are diagnosed when anxiety no longer functions as
a signal of danger or a motivation for needed change but becomes chronic and
permeates major por-tions of the person’s life, resulting in maladaptive
behav-iors and emotional disability. Anxiety disorders have many
manifestations, but anxiety is the key feature of each (American Psychiatric
Association [APA], 2000). Types of anxiety disorders include the following:
·
Agoraphobia with or without panic disorder
·
Panic disorder
·
Specific phobia
·
Social phobia
·
OCD
·
Generalized anxiety disorder (GAD)
·
Acute stress disorder
·
Posttraumatic stress disorder.
Related Topics