Chapter: Obstetric and Gynecological Nursing : Abnormal Pregnancy
Antepartum Haemorrhage
Antepartum Haemorrhage
Antepartum haemorrhage is bleeding from genital tract in late pregnancy,
after the 28 week of gestation till the end of second stage of labour.
Effect on the fetus
Fetal mortality and morbidity are increased as a result of severe
vaginal bleeding in pregnancy.
Still birth or perinatal or neonatal death may occurre Premature
placental separation and consequent hypoxia may result in the birth of a child
who is mentally and physically handiclapped.
Effect on the mother
If bleeding is severe, it may be accompanied by shock, disseminated
interavascular coagulation and renal failure. The mother may die or be left
with permanent ill- health.
Types of ante partum hemorrhage
Vaginal bleeding in late pregnancy is confined to placental separation
due to placenta praevia or placental abruption.
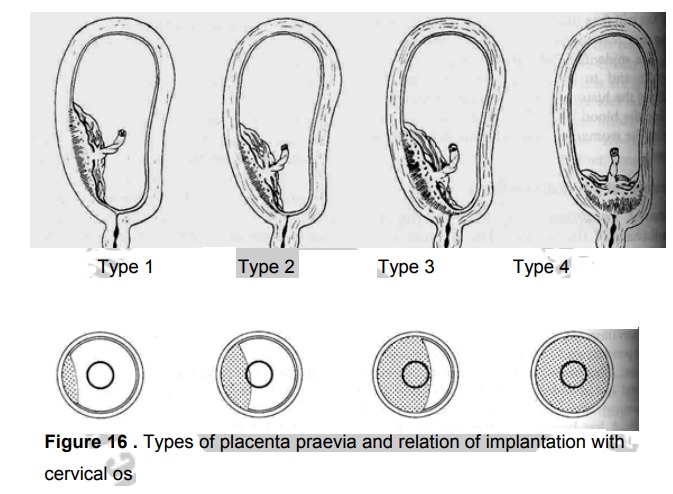
1. Placenta praevia
The placenta is partially or wholly implanted in the lower uterine
segment on either the anterior or posterior wall.
The lower uterine segment grows and stretches progressively often the 12th week of pregnancy. In late
weeks this may cause the placenta to separate and sever bleeding can occur.
Incidence- placenta pracvia occurs in 0.5% of all pregnancies.
Type 1 placenta praevia
·
The majority of the placenta is in the upper uterine segment
·
Vaginal delivery is possible
·
Blood loss is usually mild
·
The mother and the fetus remains in good condition
Type 2 placenta praevia
·
The placenta is partially located in the lower uterine segment near the
internal
·
cervical os (marginal placenta pravia).
·
Vaginal delivery is possible particularly if the placenta is implanted
anteriorly
·
Blood loss is usually moderate
·
Fetal hypoxia is more likely to be present
Type 3 placenta pracvia
·
The placenta is located centrally over the internal cervical
o
Bleeding is likely to be sever particularly when the lower segment
stretches and
·
the cervix begins to efface and dilate in late pregnancy
o
Vaginal delivery is in appropriate.
Type 4 placenta praevia
·
The placenta is located centrally over the internal cervical os and
sever haemorrhage is very likely
·
Vaginal delivery should not be considered
o
Caesarean section is essential in order to save the life of the mother
and fetus.
Sign and symptom of placenta pracvia
·
Painlessb bleedign per vagina occurs at night
·
The uterus is not tender or tense on palpation
·
The fetal head remains unengaged
·
There is malpresentation
·
The lie is oblique or transverse
·
The lie is unstable, usually in a multigravida.
Diagnosis
·
Using ultrasonic scanning will confirm the existence of placenta praevia
and establish its degree.
·
The colour of the blood is bright red, denoting fresh bleeding.
Assesement
If the haemorrhage is slight the mothers blood pressue, respiratory rate
and pulse rate may be normal In severe hemorrhage;
·
The blood pressure will be low and the pulse rate raised
·
Respirations is also rapid
·
The mother’s skin colour will be pale and her skin will be cold and
moist
·
Vaginal examination should not be attempted
Assessing the fetal condition
The mother should be asked whether fetal activity has been
normal.Excessive or cessation fetal movement is another indication of sever
fetal hypoxia.
Management of placenta praevia
The managements of placenta praevia depends on:
·
the amount of bleeding
·
the conditions of mother and fetus
·
the stage of the pregnancy
Conservative management it is appropriate if bleeding
isslight and mother and fetus are well.
·
The woman will be kept in hospital at rest until bleeding has stopped.
·
A speculum examination will have ruled out incidental causes.
·
Ultrasound scans are repeated at intervals in order to observe the
position of the placenta in relation to the cervical os.
If bleeding should occur or when the fetus is mature, an examination per
vagina will be carried out under general anesthetic at operation room. If the
placenta is felt, casearean section will be performed with out delay.
The nurse /midwife should be aware that even if vaginal delivery is
achieved, there remains a danger of postpartum haemorrhage because the placenta
has been situated in the lower segment.
Active management- sever vaginal bleeding will
necessitateimmediate delivery by caesarean section. This should take place in a
unit with facilities for special area of the new born especially if the baby
will be preterm.
Complications
·
Post partam haemorrhage
Oxytoocic drugs should be given as the baby is delivered. Occasionally
uncontrolled haemorrhage may continue and a caesarean hysterectomy may be
required.
·
Maternal shock
·
Maternal death
·
Fetal hypoxia due to placental separation
·
Fetal death
2. Placental Abruption
Placental abruption is premature separation of a normally situated
placenta occurring after the 28th week of pregnancy. The etiology of this type of
haemorrhage is not always clear, but it is often associated with pregnancy
induced hypertension or with a sudden reduction in uterine size. Rarely, direct
trauma to the abdomen may partially dislodge the placenta. Placental abruption
is an accidental occurrence of haemorrhage in 2% of all pregnancies. Partial
separation of the placenta causes bleeding from the maternal venous sinuses in
the placental bed. Further bleeding continues to separate the placenta to a
greater or lesser degree.
Types of placental abruption
The blood loss from a placenta abruption may be defined as revealed,
concealed or mixed haemorrhage. An alternative classification, based on the
degree of separation and therefore related to the condition of mother and baby
is of mild, moderate and sever haemorrhage. Concealed haemorragec is
·
Blood is retained behind the placenta.
·
The mother will have all the signs and symptoms of hypovolaemic shock.
·
Causes uterine enlargement and extreme pain.
·
The uterus appears bruised & edematous
Revealed haemorrage-blood flow to the external and no blood is
accumulated behind the placenta.
A combination of these two situations where some of the blood drains via
the vagina and some is retained behind the placenta is known as a mixed
haemorrhage
Assessment of the mother’s condition
There may be history of pregnancy induced hypertension, external
cephalic version.If there is placental separation after the birth of a first
twin or loss of copious amounts of amniotic fluid during rupture of aminiotic
memberane.
If the blood loss is revealed;
More severe degrees are associated with abdominal pain The uterus has a
hard consistency and there is a guarding on palpation of the abdomen.Fetal
parts may not be palpable the fetal heart is unlikely to be heard with a fetal
stethoscope.
Management
·
Any women with a history suggestive of placenta abruption needs urgent
medical attention. She should be transferred urgently to a consultant obstetric
unit after securing interavenous infusion.
·
Pain exacerbates shock and must be alleviated
·
Secure interavenous infusion
Observation
·
Vital sign should be recorded
·
Urinary out put is accurately assessed
·
Fluid intake must also be recorded accurately
·
If the fetus is alive, the fetal heart rate should be monitored
continuously
·
Any deterioration in the maternal or fetal condition must be immediately
reported to the obstetrician.
If the mother is not in labour and the gestation is less than 37 weeks
she may be cared for in an antenatal area for a few days and assessed for the
risks.
Mothers who have passed the 37th week of pregnancy will have an amniotomy to
induce labour. Further bleeding or evidence of fetal distress may indicate that
a caesarean section is necessary.
Moderate separation of the placenta up to 1000ml of blood may be lost
and in severe separation of the placenta about 2000ml of blood or more are lost
from the circulation.
Complications
·
Coagulations defects
·
Renal failure and pituitary failure.
·
Postpartum haemorrhage
·
Intera uterine fetal death
Related Topics