Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Kidney Disease
Anesthesia for Patients with Mild to Moderate Renal Impairment
Anesthesia for Patients with Mild to Moderate Renal Impairment
PREOPERATIVE CONSIDERATIONS
The kidney normally possesses large
functional reserve. GFR, as determined by creatinine clearance, can decrease
from 120 to 60 mL/min without any clinically perceptible change in renal
function. Even patients with creatinine clearances of 40–60 mL/min usually are
asymptomatic. These patients have only mild renal impairment but should still
be thought of as having decreased renal reserve. The emphasis in the care of
these patients is preservation of the remaining renal function, which is best
accom-plished by maintaining normovolemia and normal renal perfusion.
When
creatinine clearance decreases
to 25–40 mL/min, renal impairment is moderate, and patients are said to
have renal insufficiency. Azote-mia is always present, and hypertension and
ane-8 mia are
common. Correct anesthetic management of this group of
patients is as critical as management of those with frank kidney failure,
especially during procedures associated with a relatively high incidence of
postoperative kidney failure, such as cardiac and aortic recon-9 structive
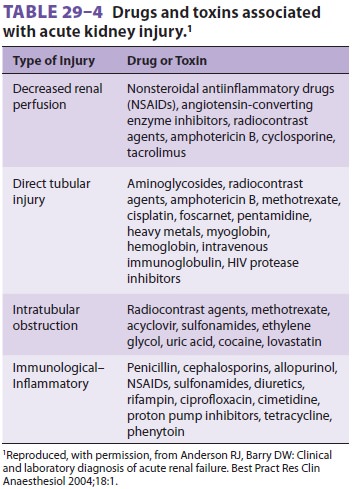
surgery. Intravascular volume depletion, sepsis, obstructive
jaundice, crush injuries, and renal toxins such as radiocontrast agents,
certain antibiotics, angiotensin-converting enzyme inhibitors, and NSAIDs (see
Table 29–4) are additional major risk factors for acute deterio-ration in
renal function. Hypovolemia
and decreased renal perfusion are particularly impor-tant causative
factors in the development of acute postoperative kidney failure. The emphasis
in man-agement of these patients is on prevention, because the mortality rate
of postoperative kidney failure may surpass 50%. The combination of diabetes and preexisting kidney disease markedly increases the
perioperative risk of renal function deterioration and of kidney failure. Renal protection with adequate hydration and maintenance of
renal blood flow is indicatedfor patients at high
risk for kidney injury and kidney failure undergoing cardiac, major aortic reconstruc-tive,
and other surgical procedures associated with significant physiological
trespass. The use of man-nitol, low-dose dopamine infusion, loop diuretics, or
fenoldopam for renal protection is controversial and without conclusive proof
of efficacy.
INTRAOPERATIVECONSIDERATIONS
Monitoring
The American Society of
Anesthesiologists’ basic monitoring standards are used for procedures involving
minimal fluid losses. For procedures asso-ciated with significant blood or
fluid loss, close mon-itoring of hemodynamic performance and urinary output is
useful . Although mainte-nance of urinary output does not ensure preserva-tion
of renal function, urinary outputs greater than 0.5 mL/kg/h are preferable.
Continuous intraarterial blood pressure monitoring is also important if rapid
changes in blood pressure are anticipated, such as in patients with poorly
controlled hypertension and in those undergoing procedures associated with
abrupt changes in sympathetic stimulation or in cardiac preload or afterload.
Induction
Selection of an induction agent is not as impor-tant as ensuring
an adequate intravascular vol-ume prior to induction; induction of anesthesia
in hypovolemic patients with renal insufficiency frequently results in
hypotension. Unless a vaso-pressor is administered, such hypotension typi-cally
resolves only following intubation or surgical stimulation. Renal perfusion,
which may already be compromised by preexisting hypovolemia, may then
deteriorate further, first as a result of hypo-tension, and subsequently from
sympathetically or pharmacologically mediated renal vasoconstric-tion. If
sustained, the decrease in renal perfusion may contribute to postoperative
renal impairment or failure. Preoperative hydration usually prevents this
sequence of events.
Maintenance of Anesthesia
All anesthetic maintenance agents are accept-able, with the
possible exception of sevoflurane administered with low gas flows over a
prolonged time period. Intraoperative deterioration in renal function may
result from adverse effects of the operative procedure (hemorrhage, vascular
occlu-sion, abdominal compartment syndrome, arterial emboli) or anesthetic
(hypotension secondary to myocardial depression or vasodilation), from
indi-rect hormonal effects (sympathoadrenal activa-tion or antidiuretic hormone
secretion), or from impeded venous return secondary to positive-pressure
ventilation. Many of these effects are almost completely avoidable or
reversible when adequate intravenous fluids are given to maintain a normal or
slightly expanded intravascular volume. The administration of large doses of
predomi-nantly α-adrenergic vasopressors (phenylephrine and norepinephrine) may
also be detrimental to preservation of renal function. Small, intermittent
doses, or brief infusions, of vasoconstrictors may be useful in maintaining
renal blood flow until other measures (eg, transfusion) are undertaken to
correct hypotension.
Fluid Therapy
As reviewed above, appropriate fluid
administration is important in managing patients with impaired renal function.
Concern over fluid overload is jus-tified, but problems are rarely encountered
in such patients with normal urinary outputs if rational fluid administration
guidelines and appropriate moni-toring are employed . The adverse consequences
of excessive fluid overload—namely, pulmonary congestion or edema—are far
easier to treat than those of AKI and kidney failure.
Related Topics