Chapter: Medicine and surgery: Cardiovascular system
Unstable angina and non-ST elevation myocardial infarction (NSTEMI) - Ischaemic heart disease
Unstable angina and non-ST elevation myocardial infarction (NSTEMI)
Definition
Acute coronary syndrome without ST elevation.
Incidence
120,000 cases in England and Wales per annum.
Clinical features
Patients present with the acute ischaemic chest pain of ACS.
Investigations
Serial ECGs are essential to exclude the development of an acute myocardial infarction (ST segment elevation or new left bundle branch block). In non-ST elevation ACS, the ECG may be normal or show ST depression and/or T wave changes corresponding to the area of the lesion. There may also be signs of hypertrophy or previous infarction (Q waves). The evolution of ECG changes is also useful for prognostic information and planning of management. Additional ECGs should also be performed during subsequent episodes of chest pain.
Twelve hours after the onset of chest pain, a troponin T or I level should be checked. If this is raised, this is diagnostic of a NSTEMI. If the level is normal patients are defined as having unstable angina.
Management
Once diagnosed with non-ST elevation ACS, all patients should be commenced on aspirin and subcutaneous low-molecular-weight heparin. Coexisting arrhythmias should be treated and oxygen given as appropriate. Continuing chest pain is treated with intravenous glyceryl trinitrate infusion. Patients should be commenced on a β-blocker (unless contraindicated) and an oral nitrate once the intravenous infusion is not required. In patients with contraindications to β-blockers, a non-dihydropyridine calcium channel antagonist, e.g. diltiazem should be used.
Patients can be stratified as to acute ischaemic risk depending on symptoms and investigations (see Table 2.5).
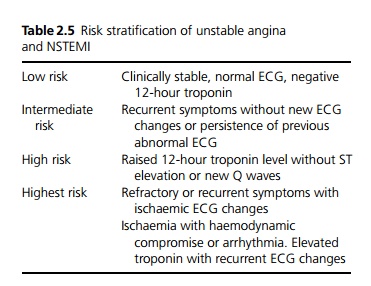
· Low-risk patients should be discharged with an elective exercise/stress test pre- or post-discharge.
· Intermediate-risk patients should have an inpatient stress or exercise test. If this shows reversible ischaemia angiography and revascularisation should be considered.
· High-risk patients may benefit from a glycoprotein IIb/IIIa inhibitor (which prevents platelet aggregation) together with unfractionated intravenous heparin in place of low-molecular-weight heparin. They should undergo inpatient angiography and revascularisation as appropriate.
· Very high risk patients should be given a glycoprotein IIb/IIIa inhibitor together with unfractionated intra-venous heparin in place of low-molecular-weight heparin and where possible undergo emergency angiography with revascularisation unless contraindicated.
Prognosis
Unless aggressively treated, approximately 10% of patients (excluding those with a normal ECG) will proceed to myocardial infarction or death within 1 month.
Related Topics