Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Mood Disorders
Treatment of Major Depression: Monoamine Oxidase Inhibitors
Monoamine Oxidase Inhibitors
Iproniazid, originally
developed for the treatment of tu-berculosis, exhibited mood-elevating
properties during clinical trials in tuberculosis patients with depression. The
distinguishing biochemical feature between iproni-azid and other chemically
similar antituberculosis com-pounds was the ability of the former to inhibit
MAO. Thus, a series of hydrazine and non–hydrazine-related MAOI agents was
synthesized and tested for antide-pressant properties. Three MAOI agents are
approved in the United States for use in major depression: isocar-boxazid (Marplan), phenelzine (Nardil), and tranyl-cypromine (Parnate).
The MAOIs are as effective as
the heterocyclic anti-depressants and the newer agents, such as the SSRIs.
However, at least two forms of life-threatening toxicity (hepatotoxicity and
dietary tyramine–induced hyper-tensive crisis ) have been associated with their
chronic use. For this reason, the MAOIs are not considered first-line agents in
the treatment of depression. They are gen-erally reserved for treatment of
depressions that resist therapeutic trials of the newer, safer antidepressants.
However, a new transdermal formulation of selegiline undergoing clinical trials
demonstrates antidepressant efficacy without concerns of liver toxicity or
dietary tyramine-induced hypertension.
Mechanism of Action
Monoamine oxidase exists in
the human body in two molecular forms, known as type A and type B. Each of
these isozymes has selective substrate and inhibitor characteristics.
Neurotransmitter amines, such as norep-inephrine and serotonin, are
preferentially metabolized by MAO-A in the brain. MAO-B is more likely to be
in-volved in the catabolism of human brain dopamine, al-though dopamine is also
a substrate for MAO-A.
Isocarboxazid, phenelzine,
and tranylcypromine are irreversible nonselective inhibitors of both MAO-A and
MAO-B. However, it appears that inhibition of MAO-A, not MAO-B, is important to
the antidepres-sant action of these agents.
Therapeutic efficacy by
selective MAO-A inhibitors (such as clorgyline or moclobemide) in major
depres-sions strongly suggests that MAO inhibition at central serotonin or
norepinephrine synapses or both is re-sponsible for the antidepressant
properties of these agents. However, since complete MAO-A inhibition is
achieved clinically within a few days of treatment, while the antidepressant
effects of these drugs are not ob-served for 2 to 3 weeks, suggests that additional
actions must be involved.
In a manner similar to that
of the TCAs and SSRIs, MAOIs are known to induce adaptive changes in the CNS
synaptic physiology over 2 to 3 weeks. These changes result in both
down-regulation of synaptic transmission mediated through noradrenergic α- and β- adrenoceptors and
up-regulation or enhancement of synaptic transmission at serotonin synapses
(5HT1A-receptors). This action on serotonin neurotransmission is the
result of desensitized somatodendritic autorecep-tors responsible for the
regulation of the firing rate of serotonin-containing neurons of the forebrain.
Accordingly, these neurons fire at elevated rates, releas- ing large quantities
of serotonin into the synapse. This serotonin is protected from degradation by
inhibition of synaptic MAO-A. It is believed that the development of these
physiological changes at norepinephrine and serotonin synapses, which parallel
the time delay asso-ciated with the antidepressant properties of the MAOIs, is
the mechanism of action for these agents in the treat-ment of major depression.
Adverse Effects
The potential for toxicity
that is associated with the ad-ministration of the MAOIs restricts their use in
major depression. Hepatotoxicity is likely to occur with iso-carboxazid or
phenelzine, since hydrazine compounds can cause damage to hepatic parenchymal
cells. This is true particularly for patients identified as slow
acetyla-tors of hydrazine compounds.
For-tunately, the incidence of hepatotoxicity is low with the available agents.
A greater concern is the
potentially lethal cardio-vascular effects that can occur in patients who do
not comply with their dietary restrictions. Patients who take a MAOI should not
eat food rich in tyramine or other biologically active amines. Normally, these
amines are rapidly metabolized by MAO-A during gastric absorp-tion by the
mucosal cells of the intestinal wall and by MAO-A and MAO-B during passage
through the liver parenchyma. If both isozymes of MAO are inhibited, el-evated
circulating levels of tyramine will be free to in-teract with the sympathetic
noradrenergic nerve termi-nals innervating cardiac and vascular smooth muscle
tissue to produce a pressor effect . In these conditions, tyramine can cause an
acute elevation in blood pressure, sometimes leading to a hypertensive crisis.
Cheeses, wine, and a whole host of other foods rich in tyramine must be
avoided. A number of other bothersome side effects, such as tremors,
orthostatic hy-potension, ejaculatory delay, dry mouth, fatigue, and weight gain,
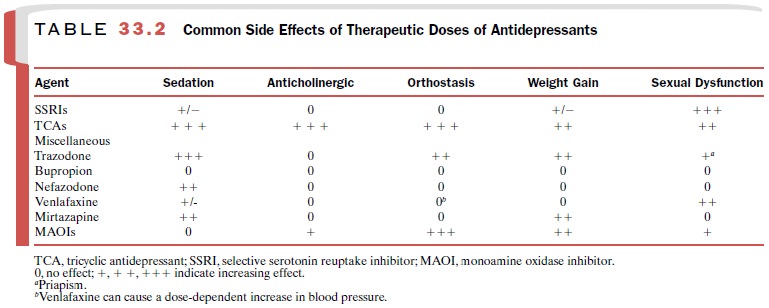
are common at therapeutic doses of MAOIs (Table 33.2).
Drug Interactions
Serious hypertension can
occur with concomitant ad-ministration of over-the-counter cough and cold
med-ications containing sympathomimetic amines. When switching from a MAOI to
another antidepressant, such as a SSRI, a drug-free period of 2 weeks is
required to allow for the regeneration of tissue MAO and elimina-tion of the
MAOI. When switching from an antidepres-sant, such as an SSRI, to a MAOI,
sufficient time should be allowed for the SSRI to be cleared from the body (at
least 5 half-lives) before starting the MAOI. Special note should be taken of
fluoxetine’s long half-life, re-quiring at least 5 weeks after discontinuation
of fluoxe-tine at a 20-mg dose and longer at higher doses, before initiation of
MAOI therapy. Coadministration of a MAOI and an SSRI or venlafaxine can
overstimulate the serotonin receptors in the brainstem and spinal cord
(serotonin syndrome), which can be lethal. Serotonin syndrome consists of a
constellation of psychiatric, neu-rological, and cardiovascular symptoms that
may in-clude confusion, elevated or dysphoric mood, tremor, myoclonus,
incoordination, hyperthermia, and cardio-vascular collapse.
Related Topics