Chapter: Medicine and surgery: Cardiovascular system
Systemic hypertension - Hypertension and vascular diseases
Hypertension and vascular diseases
Systemic hypertension
Definition
Hypertension means high blood pressure (BP). The World Health Organisation latest guidelines define hypertension with three grades of severity that reflect the fact that systolic and diastolic hypertension are independent risk factors for complications of hypertension:
Grade 1 (mild): A systolic BP of Ōēź140 mmHg or a diastolic BP of Ōēź90 mmHg.
Grade 2 (moderate): A systolic BP of Ōēź160 mmHg or a diastolic BP of Ōēź100 mmHg.
Grade 3 (severe): A systolic BP of Ōēź180 mmHg or a diastolic BP of Ōēź110 mmHg.
Incidence
Common. Up to 25% of the adult population is hypertensive by these criteria.
Age
Increases with age (>50% affected over the age of 65 years).
Sex
M > F
Geography
Rising prevalence of hypertension in the developing world, together with longer life expectancies, is increasing the morbidity of complications.
Aetiology
Divided into primary (essential) and secondary hypertension:
Essential hypertension (>90%)
┬Ę Non-modifiable: Genetic (racial and familial), gender (males higher).
┬Ę Modifiable: Obesity, alcohol intake, diet (especially high salt intake).
Secondary hypertension (<10%)
┬Ę Renal (80%): Most commonly glomerulonephritis, recurrent/chronic pyelonephritis, and polycystic kidneys. Hypertension is also a common cause of renal disease.
┬Ę Endocrine causes: Acromegaly, CushingŌĆÖs syndrome, ConnŌĆÖs syndrome and phaechromocytoma.
┬Ę Cardiovascular (uncommon): Coarctation of the aorta, renal artery stenosis.
┬Ę Pregnancy (pre-eclampsia).
┬Ę Drugs: Oral contraceptives, NSAIDs, steroids. Car-benoxalone and liquorice mimic aldosterone.
Pathophysiology
┬Ę Hypertension accelerates the agerelated process of arteriosclerosis ŌĆśhardening of the arteriesŌĆÖ and predisposes to atherosclerosis in larger arteries. Arteriosclerosis, through smooth muscle hypertrophy and intimal thickening, reduces luminal diameter in smaller arteries and so increases peripheral vascular resistance and exacerbates hypertension.
┬Ę The chronic increased pressure load on the heart results in left ventricular hypertrophy and over time this leads to heart failure.
┬Ę Arteriosclerosis also reduces renal perfusion pressure, which activates the reninŌĆōangiotensin system. Salt and water retention occurs, which can itself worsen hyper-tension.
In some individuals the pressure rise is more rapid and such patients are said to have malignant hypertension (with rapidly worsening end-organ damage such as hypertensive retinopathy and renal impairment). Without treatment these patients die within 1ŌĆō2 years.
Clinical features
As blood pressure varies considerably (e.g. diurnal variation, recent alcohol intake, stress and anxiety) the diagnosis should be based on multiple measurements taken on several different occasions. These should be taken with the patient relaxed and at rest. In cases of doubt, 24-hour blood pressure recordings may be helpful such as when ŌĆśwhite coatŌĆÖ hypertension is suspected.
A full history and examination should be performed to assess the extent, to look for any underlying cause or contributing factors and to look for complications. Often hypertension is asymptomatic and the history and examination are unremarkable.
Complications
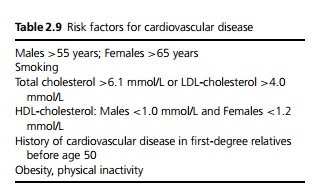
Hypertension is a major risk factor for cerebrovascular disease (strokes), heart disease (coronary artery disease, left ventricular hypertrophy and heart failure) (see Table 2.9) and renal failure. Other important complications include peripheral vascular disease and dissecting aortic aneurysms.
In patients with malignant hypertension there is risk of cerebral oedema, left ventricular failure, renal impairment with proteinuria and microscopic haematuria. In severe hypertension, retinal haemorrhages, exudates and papilloedema are features of malignant hypertension.
Macroscopy/microscopy
Benign hypertension and small arteries: There is hypertrophy of the muscular media, thickening of the elastic lamina, fibroelastic thickening of the intima and reduction in the size of the lumen.
Malignant hypertension and small arteries: Loose myxomatous intimal proliferation with reduced lumen and normal media.
Arterioles: There is hyaline wall thickening (hyaline arteriosclerosis), increased rigidity and reduced lumen size.
Malignant hypertension and arterioles: Fibrinoid necrosis is seen in the walls of arterioles.
Investigations
Routine investigations must include fasting plasma glucose, serum total cholesterol and lipid profile, U&Es, FBC, urinalysis (dipstick), ECG and serum uric acid.
Other tests may include echocardiogram, carotid ultrasound, microalbuminuria (essential test in diabetics), quantitative proteinuria (if dipstick test positive) and fundoscopy in severe hypertension.
Specialist tests include further tests for end organ damage (cerebral, cardiac renal) and tests for the causes of secondary hypertension (renin, aldosterone, corticosteroids, catecholamines, arteriography, renal and adrenal ultrasound, MRI brain).
Management
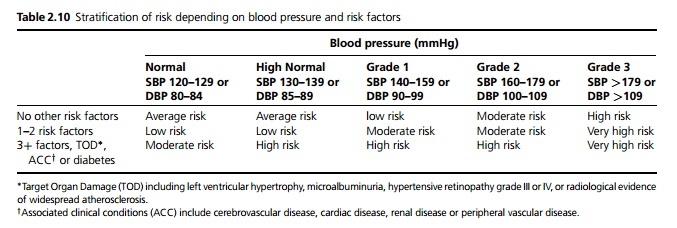
Treatment is based on the total level of cardiovascular risk and the level of systolic and diastolic blood pressure (see Tables 2.9 and 2.10)
┬Ę All patients should be advised to have lifestyle changes, including weight reduction, alcohol limitation, salt re-striction, reduced total and saturated fat intake and increased fruit and vegetable consumption and increased exercise. Stopping smoking as well as the actions mentioned above will also reduce overall cardio-vascular risk.
┬Ę Patients with high or very high risk should begin treatment immediately. Patients with moderate risk should remain under close followup. If after 3 months their systolic blood pressure is above 139 or the diastolic above 89, treatment should be started. The remainder of patients and those with low or average risk should remain under long-term follow-up.
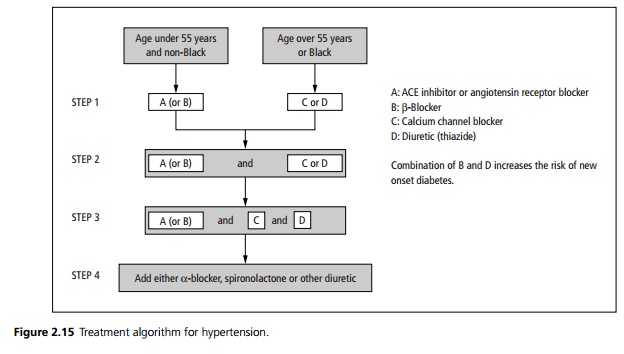
┬Ę Combination drug treatment is often required. A treatment algorithm is shown in Fig. 2.15.
Prognosis
Patients with untreated malignant hypertension have a 1-year mortality rate of 90%. In general the risks from hypertension are dependent on:
┬Ę The level of blood pressure,
┬Ę Presence of retinal changes, presence of renal or cardiac impairment,
┬Ę Being male is a greater risk than female,
┬Ę Age (young fare worse than old) and
┬Ę Coexistence of coronary disease and risk factors.
Related Topics