Chapter: Clinical Dermatology: Eczema and dermatitis
Seborrhoeic eczema
Seborrhoeic
eczema
Presentation and course
The
term covers at least three common patterns of eczema, mainly affecting hairy
areas, and often show-ing characteristic greasy yellowish scales. These
pat-terns may merge together (Fig. 7.19).
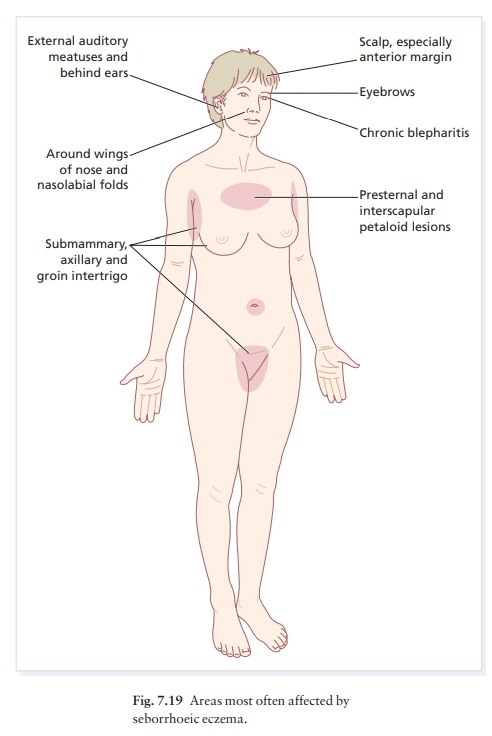
1.
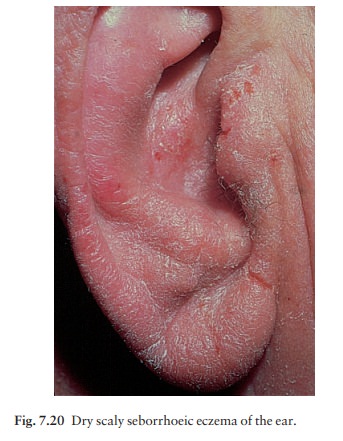
A red scaly or exudative eruption of the scalp, ears (Fig. 7.20), face (Fig.
7.21) and eyebrows. May be associated with chronic blepharitis and otitis
externa.

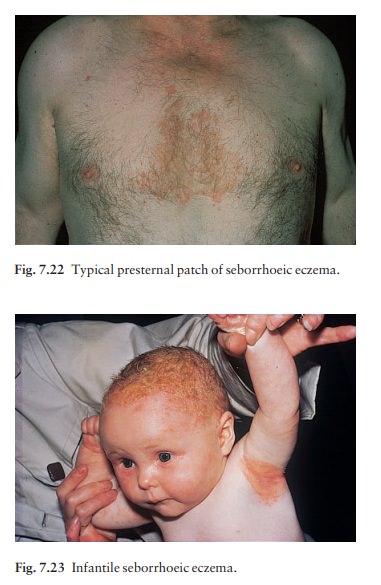
2. Dry scaly
‘petaloid’ lesions of the presternal(Fig. 7.22) and interscapular areas. There
may also be extensive follicular papules or pustules on the trunk (seborrhoeic
folliculitis or pityrosporum folliculitis).
3 Intertriginous
lesions of the armpits, umbilicus or groins, or under spectacles or hearing
aids.
Cause
This
condition is not obviously related to seborrhoea. It may run in some families,
often affecting those with a tendency to dandruff. The success of treatments
directed against yeasts has suggested that overgrowth of the pityrosporum yeast
skin commensals plays an important part in the development of seborrhoeic
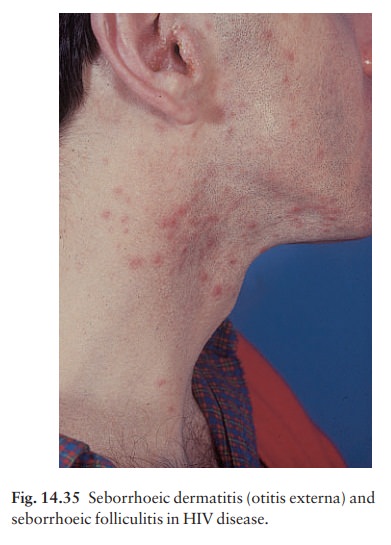
eczema. This fits well with the fact that seborrhoeic eczema is often an early
sign of AIDS, and that it responds to antiyeast agents such as topical
ketocona-zole shampoo or cream.
Seborrhoeic
eczema may affect infants (Fig. 7.23) but is most common in adult males. In
infants it clears quickly but in adults its course is unpredictable and may be
chronic or recurrent. Some particularly severe cases have occurred in patients
with AIDS (Fig. 14.35).
Complications
May
be associated with furunculosis. In the intertriginous type, superadded Candida
infection is common.
Investigations
None
are usually needed, but bear possible HIV infection and Parkinson’s disease in
mind.
Treatment
Therapy
is suppressive rather than curative and patients should be told this. Topical
imidazoles are perhaps the first line of treatment. Two per cent sulphur and 2%
salicylic acid in aqueous cream is often helpful and avoids the problem of
topical steroids. It may be used on the scalp overnight and removed by a
medicated shampoo, which may con-tain ketoconazole, tar, salicylic acid,
sulphur, zinc or selenium sulphide. A topical lithium preparation may help the facial rash. For intertriginous
lesions a weak steroid–antiseptic or steroid–antifungal combination is often effective. For severe and
unresponsive cases a short course of oral itraconazole may be helpful.
Related Topics