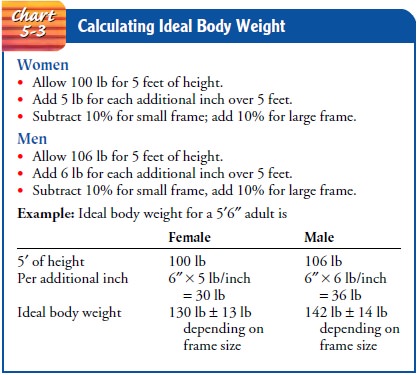
Chapter: Medical Surgical Nursing: Health Assessment
Physical Health Assessment
Physical Assessment
Physical assessment, or
the physical examination, is an integral part of nursing assessment. The basic
techniques and tools used in performing a physical examination. The examination
of specific systems, including spe-cial maneuvers. Because the patient’s
nutritional status is an important factor in health and well-being.
The physical examination
is usually performed after the health history is obtained. It is carried out in
a well-lighted, warm area. The patient is asked to undress and draped
appropriately so that only the area to be examined is exposed. The person’s
physical and psychological comfort is considered at all times. Procedures and
sensations to expect are described to the patient before each part of the
examination. The examiner’s hands are washed before and immediately after the
examination. Fingernails are kept short to avoid injuring the patient. The
examiner wears gloves when there is a possibility of coming into contact with
blood or other body secretions during the physical examination.
An organized and
systematic examination is the key to obtain-ing appropriate data in the
shortest time. Such an approach en-courages cooperation and trust on the part
of the patient. The individual’s health history provides the examiner with a
health pro-file that guides all aspects of the physical examination. Although
the sequence of physical examination depends on the circum-stances and on the
patient’s reason for seeking health care, the complete examination usually
proceeds as follows:
· Skin
· Head and neck
· Thorax and lungs
· Breasts
· Cardiovascular system
· Abdomen
· Rectum
· Genitalia
· Neurologic system
· Musculoskeletal system
In clinical practice,
all relevant body systems are tested through-out the physical examination, not
necessarily in the sequence de-scribed (Weber & Kelley, 2003). For example,
when the face is examined, it is appropriate to check for facial asymmetry and,
thus, for the integrity of the seventh cranial nerve; the examiner does not
need to repeat this as part of a neurologic examination. When sys-tems are
combined in this manner, the patient does not need to change positions
repeatedly, which can be exhausting and time-consuming.
A “complete” physical
examination is not routine. Many of the body systems are selectively assessed
on the basis of the individ-ual’s presenting problem. If, for example, a
healthy 20-year-old college student requires an examination to play basketball
and re-ports no history of neurologic abnormality, the neurologic assess-ment
is brief. Conversely, a history of transient numbness and diplopia (double
vision) usually necessitates a complete neurologic investigation. Similarly, a
person with chest pain receives a much more intensive examination of the chest
and heart than the per-son with an earache. In general, the individual’s health
history guides the examiner in obtaining additional data for a complete picture
of the patient’s health.
The process of learning
physical examination requires repeti-tion and reinforcement in a clinical
setting. Only after basic physical assessment techniques are mastered can the
examiner tailor the routine screening examination to include thorough
assess-ments of a particular system, including special maneuvers.
The basic tools of the
physical examination are vision, hearing, touch, and smell. These human senses
may be augmented by spe-cial tools (eg, stethoscope, ophthalmoscope, and reflex
hammer) that are extensions of the human senses; they are simple tools that
anyone can learn to use well. Expertise comes with practice, and sophistication
comes with the interpretation of what is seen and heard. The four fundamental
techniques used in the physical ex-amination are inspection, palpation,
percussion, and auscultation (Weber & Kelley, 2003).
INSPECTION
The first fundamental
technique is inspection or observation. General inspection begins with the
first contact with the patient. Introducing oneself and shaking hands provide
opportunities for making initial observations: Is the person old or young? How
old? How young? Does the person appear to be his or her stated age? Is the
person thin or obese? Does the person appear anxious or depressed? Is the
person’s body structure normal or abnormal? In what way, and how different from
normal? It is essential to pay attention to the details in observation. Vague,
general statements are not a substitute for specific descriptions based on
careful ob-servation; for example:
· “The person appears
sick.” In what way does he or she ap-pear sick? Is the skin clammy, pale,
jaundiced, or cyanotic; is the person grimacing in pain; is breathing
difficult; does he or she have edema? What specific physical features or
be-havioral manifestations indicate that the person is “sick”?
· “The person appears
chronically ill.” In what way does he or she appear chronically ill? Does the
person appear to have lost weight? People who lose weight secondary to
muscle-wasting diseases (eg, AIDS, malignancy) have a dif-ferent appearance
than those who are merely thin, and weight loss may be accompanied by loss of
muscle mass or atrophy. Does the skin have the appearance of chronic
ill-ness—that is, is it pale, or does it give the appearance of de-hydration or
loss of subcutaneous tissue? These important observations are documented in the
patient’s chart or health record.
Among general
observations that should be noted in the ini-tial examination of the patient
are posture and stature, body movements, nutrition, speech pattern, and vital
signs.
Posture and Stature
The posture that a
person assumes often provides valuable infor-mation about the illness. Patients
who have breathing difficulties (dyspnea) secondary to cardiac disease prefer
to sit and may re-port feeling short of breath lying flat for even a brief
time. People with obstructive pulmonary disease not only sit upright but also
may thrust their arms forward and laterally onto the edge of the bed (tripod
position) to place accessory respiratory muscles at an optimal mechanical
advantage. Those with abdominal pain due to peritonitis prefer to lie perfectly
still; even slight jarring of the bed will cause agonizing pain. In contrast,
patients with abdom-inal pain due to renal or biliary colic are often restless
and may pace the room. Patients with meningeal irritation may experience head
or neck pain on bending the head or flexing their knees
Body Movements
Abnormalities of body
movement may be of two general kinds: generalized disruption of voluntary or
involuntary movement, and asymmetry of movement. The first category includes
tremors of a wide variety; some tremors may occur at rest (Parkinson’s
disease), whereas others occur only on voluntary movement (cerebellar ataxia).
Other tremors may exist during both rest and activity (alcohol withdrawal
syndrome, thyrotoxicosis). Some voluntary or involuntary movements are fine,
others quite coarse. At the extreme are the convulsive movements of epilepsy or
tetanus and the choreiform (involuntary and irregular) movements of patients
with rheumatic fever or Huntington’s disease. Other aspects of body movement
that are noted on inspection include spasticity, muscle spasms, and an abnormal
gait.
Asymmetry of movement,
in which only one side of the body is affected, may occur with disorders of the
central nervous sys-tem (CNS), principally in those patients who have had
cerebro-vascular accidents (strokes). The patient may have drooping of one side
of the face, weakness or paralysis of the extremities on one side of the body,
and a foot-dragging gait. Spasticity (in-creased muscle tone) may also be
present, particularly in patients with multiple sclerosis.
Nutrition
Nutritional status is
important to note. Obesity may be gener-alized as a result of excessive intake
of calories or may be specif-ically localized to the trunk in those with
endocrine disorders (Cushing’s disease) or those who have been taking
cortico-steroids for long periods of time. Loss of weight may be gener-alized
as a result of inadequate caloric intake or may be seen in loss of muscle mass
with disorders that affect protein synthesis.
Speech Pattern
Speech may be slurred
because of CNS disease or because of dam-age to cranial nerves. Recurrent
damage to the laryngeal nerve will produce hoarseness, as will disorders that
produce edema or swelling of the vocal cords. Speech may be halting, slurred,
or in-terrupted in flow in some CNS disorders (eg, multiple sclerosis).
Vital Signs
The recording of vital
signs is a part of every physical examina-tion. Blood pressure, pulse rate,
respiratory rate, and body tem-perature measurements are obtained and recorded.
Acute changes and trends over time are documented; unexpected changes and
values that deviate significantly from the patient’s normal values are brought
to the attention of the patient’s primary health care provider. The “fifth
vital sign,” pain, is also assessed and docu-mented, if indicated.
Fever is an increase in body temperature above normal. A nor-mal oral temperature for most people is an average of 37.0°C (98.6°F); however, some variation is normal. Some people’s tem-peratures are quite normal at 36.6°C (98°F) and others at 37.3°C (99°F). There is a normal diurnal variation of a degree or two in body temperature throughout the day; with temperature usually lowest in the morning and rising during the day to between 37.3° and 37.5°C (99° to 99.5°F), then decreasing again during the night.
PALPATION
Palpation is a vital
part of the physical examination. Many struc-tures of the body, although not
visible, may be assessed through the techniques of light and deep palpation
(Fig. 5-3). Examples include superficial blood vessels, lymph nodes, the
thyroid, the organs of the abdomen and pelvis, and the rectum. When the
ab-domen is examined, auscultation is performed before palpation and percussion
to avoid altering bowel sounds.
Sounds generated within
the body, if within specified fre-quency ranges, also may be detected through
touch. Thus, cer-tain murmurs generated in the heart or within blood vessels
(thrills) may be detected. Thrills cause a sensation to the hand much like the
purring of a cat. Voice sounds are transmitted along the bronchi to the
periphery of the lung. These may be per-ceived by touch and may be altered by
disorders affecting the lungs. The phenomenon is called tactile fremitus and is useful in assessing diseases of the chest.
PERCUSSION
The technique of percussion (Fig. 5-4) translates the application of physical force into sound. It is a skill requiring practice but one that yields much information about disease processes in the chest and abdomen. The principle is to set the chest wall or abdominal wall into vibration by striking it with a firm object. The sound produced reflects the density of the underlying structure. Certain densities produce sounds as percussion notes.
These sounds, listed in a sequence that proceeds
from the least to the most dense, are called tympany, hyperresonance,
resonance, dullness, and flatness. Tym-pany is the drumlike sound produced by
percussing the air-filled stomach. Hyperresonance is audible when one percusses
over in-flated lung tissue in someone with emphysema. Resonance is the sound
elicited over air-filled lungs. Percussion of the liver produces a dull sound,
whereas percussion of the thigh results in flatness.
Percussion allows the
examiner to assess such normal anatomic details as the borders of the heart and
the movement of the di-aphragm during inspiration. One may determine the level
of pleural effusion (fluid in the pleural cavity) and the location of a
consolidated area caused by pneumonia or atelectasis (collapse) of a lobe of
the lung. The use of percussion is described further with disorders of the
thorax and abdomen.
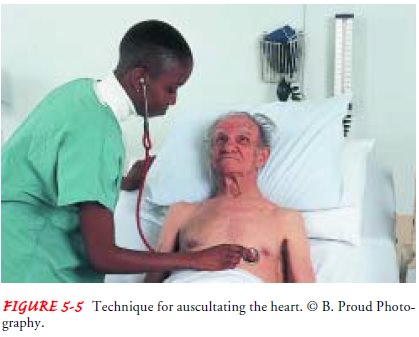
AUSCULTATION
Auscultation is the
skill of listening to sounds produced within the body created by the movement
of air or fluid. Examples in-clude breath sounds, the spoken voice, bowel
sounds, cardiac murmurs, and heart sounds. Physiologic sounds may be normal
(eg, first and second heart sounds) or pathologic (eg, heart mur-murs in
diastole, or crackles in the lung). Some normal sounds may be distorted by
abnormalities of structures through which the sound must travel (eg, changes in
the character of breath sounds as they travel through the consolidated lung of
the patient with lobar pneumonia).
Sound produced within
the body, if of sufficient amplitude, may be detected with the stethoscope,
which functions as an ex-tension of the human ear and channels sound. Two end
pieces are available for the stethoscope: the bell and the diaphragm. The bell
is used to assess very-low-frequency sounds such as diastolic heart murmurs.
The entire surface of the bell’s disc is placed lightly on the skin surface to
avoid flattening the skin and reducing audible vibratory sensations. The
diaphragm, the larger disc, is used to as-sess high-frequency sounds such as
heart and lung sounds and is held in firm contact with the skin surface (Fig.
5-5). Touching the tubing or rubbing other surfaces (hair, clothing) during
ausculta-tion is avoided to minimize extraneous noises.
Sound produced by the body, like any other sound, is charac-terized by intensity, frequency, and quality. Intensity, or loudness, associated with physiologic sound is low; thus, the use of the stethoscope is needed.
Frequency, or pitch, of physiologic
sound is in reality “noise” in that most sounds consist of a frequency spectrum
as opposed to the single-frequency sounds that we as-sociate with music or the
tuning fork. The frequency spectrum may be quite low, yielding a rumbling
noise, or comparatively high, producing a harsh or blowing sound. Quality of sound re-lates to overtones
that allow one to distinguish between different sounds. Sound quality enables
the examiner to distinguish be-tween the musical quality of high-pitched
wheezing and the low-pitched rumbling of a diastolic murmur.
Related Topics