Chapter: Medicine and surgery: Cardiovascular system
Peripheral arterial disease - Hypertension and vascular diseases
Peripheral arterial disease
Definition
Peripheral arterial disease describes a spectrum of pathological processes affecting either the larger arteries or small vessels.
Incidence
Very common.
Age
Mainly over 50 years
Sex
M > F
Geography
More common in the Western world.
Aetiology/pathophysiology
Atheromatous plaques form especially in larger vessels at areas of haemodynamic stress such as at the bifurcation of vessels and origins of branches. It may affect younger patients, particularly diabetics and smokers.
Arteriosclerosis, ŌĆśhardening of the arteriesŌĆÖ, is an age-related condition accelerated by hypertension. It often occurs in conjunction with atheroma.
In larger arteries fibrosis of the muscular or elastic media weakens the wall and the vessel lumen enlarges. This can lead to ŌĆśunfolding of the aortaŌĆÖ and aortic regurgitation.
In smaller arteries and arterioles, the predominant effects are smooth muscle hypertrophy and intimal thickening forming concentric layers of collagen, causing luminal narrowing.
Clinical features
Chronic peripheral arterial disease in the lower limbs causes intermittent cramp-like pain in the muscles during exercise and is relieved by rest ŌĆō so-called intermittent claudication. With increasing severity of ischaemia the claudication distance falls. Severe claudication may be associated with non-healing leg ulcers that progress to gangrene. Eventually the patient develops pain at rest and this indicates critical arterial insufficiency and is a surgical emergency.
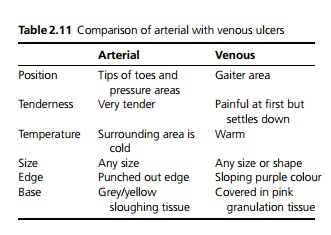
On examination, signs include cool, dry skin with loss of hair, thready or absent pulses in the affected areas and a lack of venous filling. There is often discolouration, i.e. pallor or a dark hue due to slow circulation. In advanced cases there is ulceration (see Table 2.11) or even gangrene. There may be aneurysms (e.g. abdominal or popliteal) and bruits should be listened for.
Hypertension may be the underlying cause or may be secondary to renal artery stenosis caused by atheroma.
The underlying processes are common to the entire arterial tree, therefore associated symptoms and signs should be elicited, e.g. chest pain, transient ischaemic attacks, impotence (due to internal iliac artery disease).
Complications
Gangrene and loss of limbs. Diabetics are at particular risk due to diabetic neuropathy, which allows ulcera-tion, trauma and infection to progress without pain.
Acute arterial occlusion due to thrombus or emboli from the heart or a larger vessel may cause pain, pallor, paraesthesia and paralysis, which is a surgical emergency.
Investigations
X-ray may show calcification of the vessels in the leg. Doppler ultrasound to measure ankle systolic blood
pressure and assess blood flow.
Arteriography or digital subtraction angiography allows visualisation of the arterial tree.
Management
Risk factors should be modified where possible, stopping smoking in particular may prevent further deterioration and improves symptoms in many cases. Care should be taken to avoid trauma. Exercise should be encouraged as it improves collateral supply.
Low-dose aspirin should be used to reduce risk of thromboembolism.
In most patients clinical symptoms are static or fluctuate, so conservative care is sufficient. There are four options for persistently severe symptoms. Arterioscle-rosis in older patients is difficult to treat surgically, as the vessels are small.
┬Ę Sympathectomy reduces vasospasm. It is useful to relieve rest pain in small vessel disease. It can be done percutaneously with an injection of phenol.
┬Ę Percutaneous angioplasty is most useful for short stenoses or occlusions in mediumsized arteries such as the iliac, femoral and renal arteries; however, as patients often present late the disease may be too widespread. A guide wire is inserted and then a balloon fed over the wire and inflated within the lesion. Stents are often used to improve patency. Complications include restenosis, dissection or thrombosis.
┬Ę Arterial reconstruction is preferably reserved for critical ischaemia or severely limiting intermittent claudication, because failed grafting worsens symp-toms and repeat surgery is very difficult. In addition, most patients have other conditions such as ischaemic heart disease, diabetes and cerebrovascular disease, which increases peri- and postoperative morbidity and mortality. Procedures include i) femoropopliteal grafts using saphenous vein, or polytetrafluorethylene (PTFE) and ii) more distal disease is best treated with a bypass graft from the common femoral artery to the popliteal or tibial artery as the stenosis or occlusion is usually long.
┬Ę Amputation: vascular disease causes more than 90% of all amputations; however, most vascular disease does not result in this. The level of amputation is dependent on blood supply, state of joints, general health and age. Conservation of the knee joint is important (possible in 50%) for prosthesis and walking. Normally the stump is closed by primary suture.
Prognosis
Five-year patency rates with femorodistal bypass vary between 30 and 50%, aortoiliac reconstruction has a patency rate of 80%. The most common cause of death perioperatively and during long-term follow-up is ischaemic heart disease.
Related Topics